Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-088
High Risk left Main Intervention in an Octogenarian
By Punish Sadana
Presenter
Punish Sadana
Authors
Punish Sadana1
Affiliation
Max Super Specialty Hospital, India1,
View Study Report
TCTAP C-088
Coronary - Complex PCI - Left main
High Risk left Main Intervention in an Octogenarian
Punish Sadana1
Max Super Specialty Hospital, India1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 86 year old male a known case of hypertension,Diabetes Mellitus presented in other hospital with complaints of chest pain on exertion for 3-4 monts ,increased for 10-15 days.Came to our hospital for further management.Physical examinationPulse rate 88/min,BP 116/64mmhgChest-B/l ClearCVS S1S2 normal,no murmurP/A -soft,normal bowel sounds
Relevant Test Results Prior to Catheterization
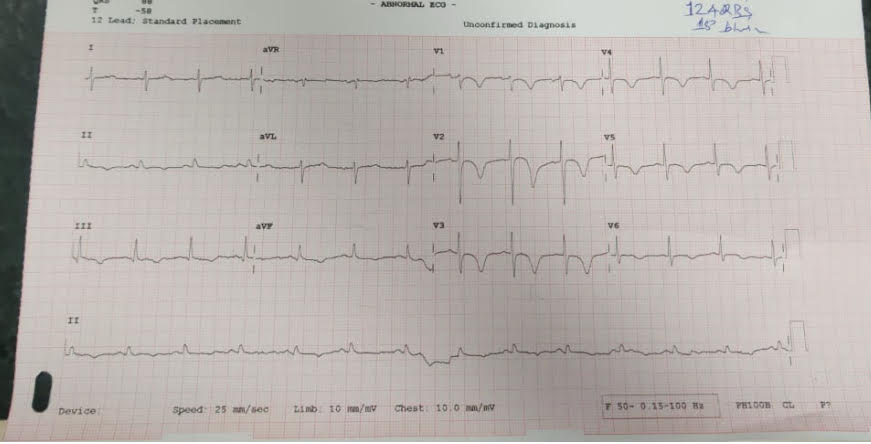
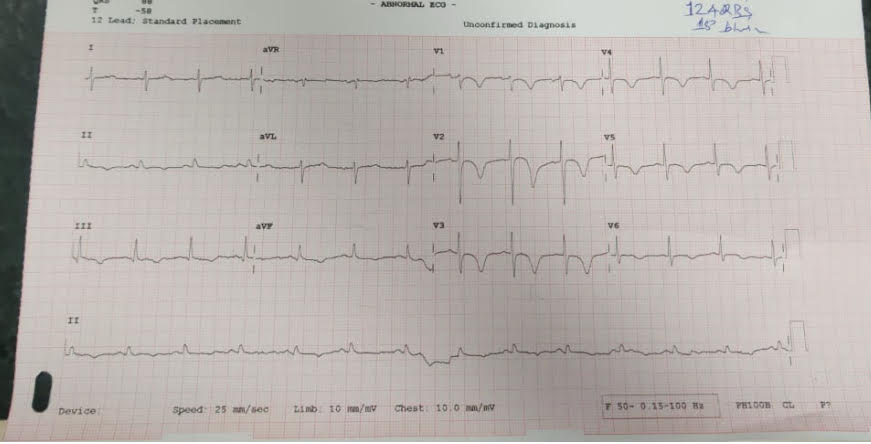
ECG-t inversion anterior and inferior leads Echo: Global hypokinesis,LVEF 45%HB 9.8Creatinine 1.5
Relevant Catheterization Findings
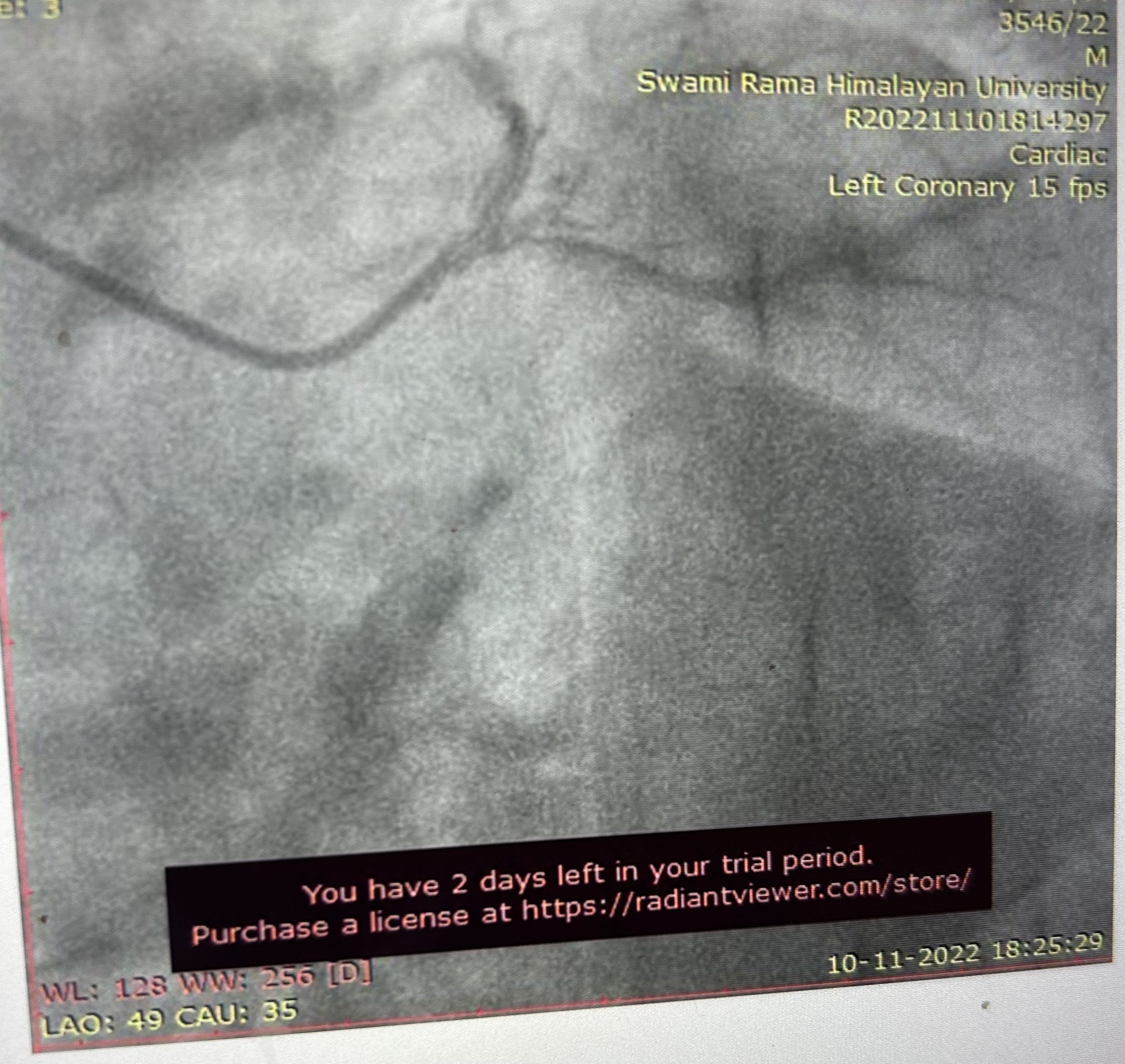
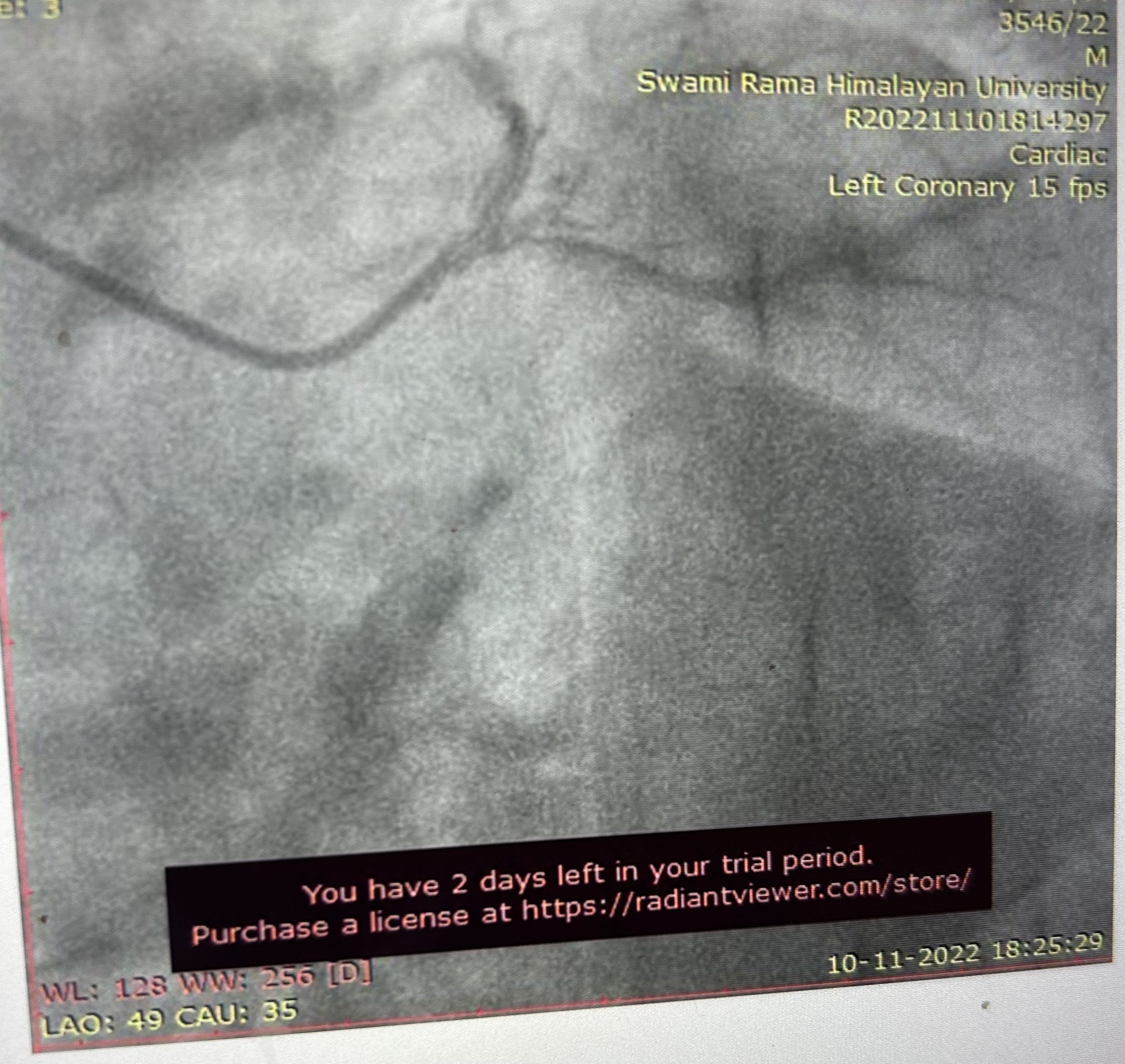
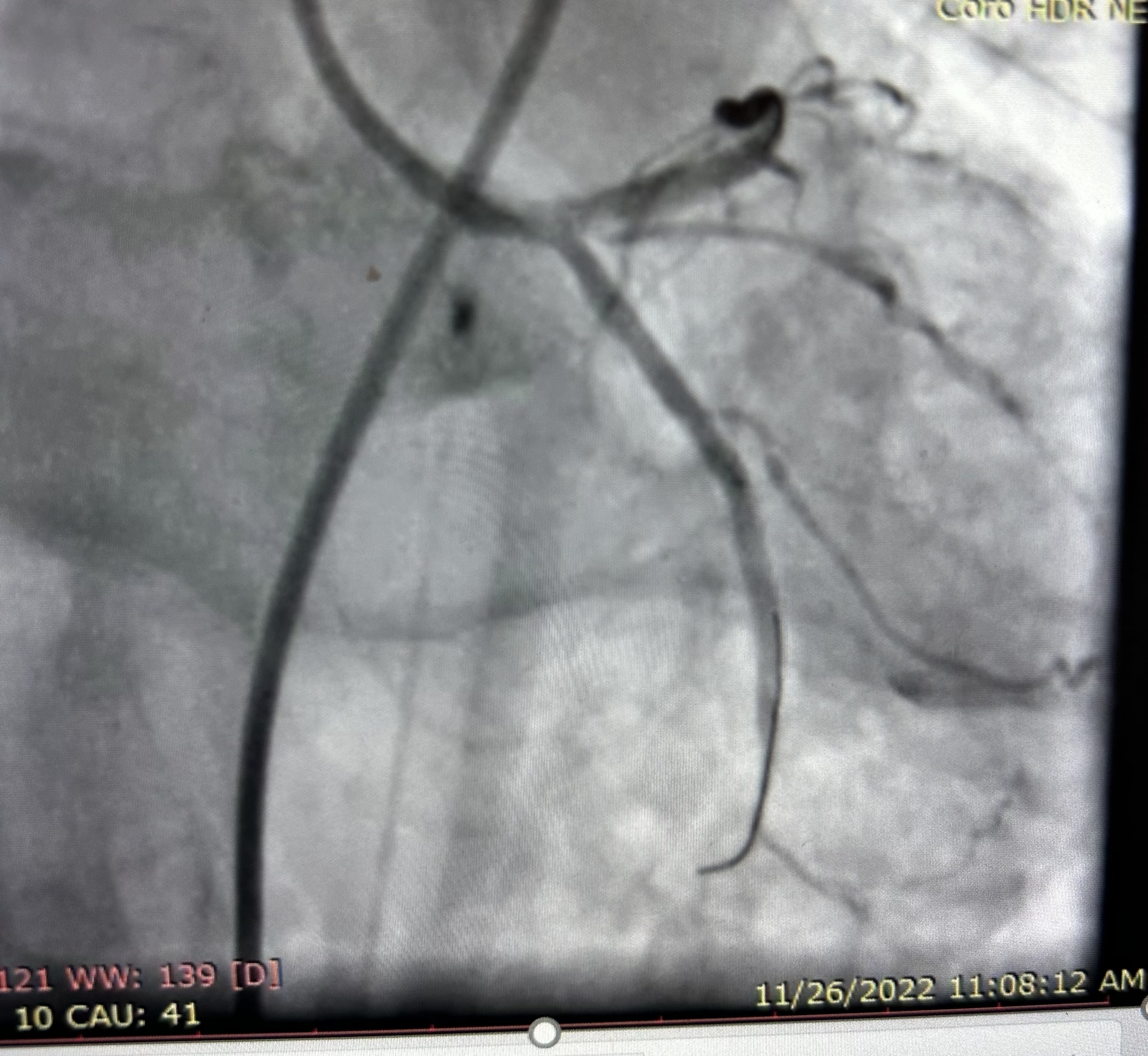
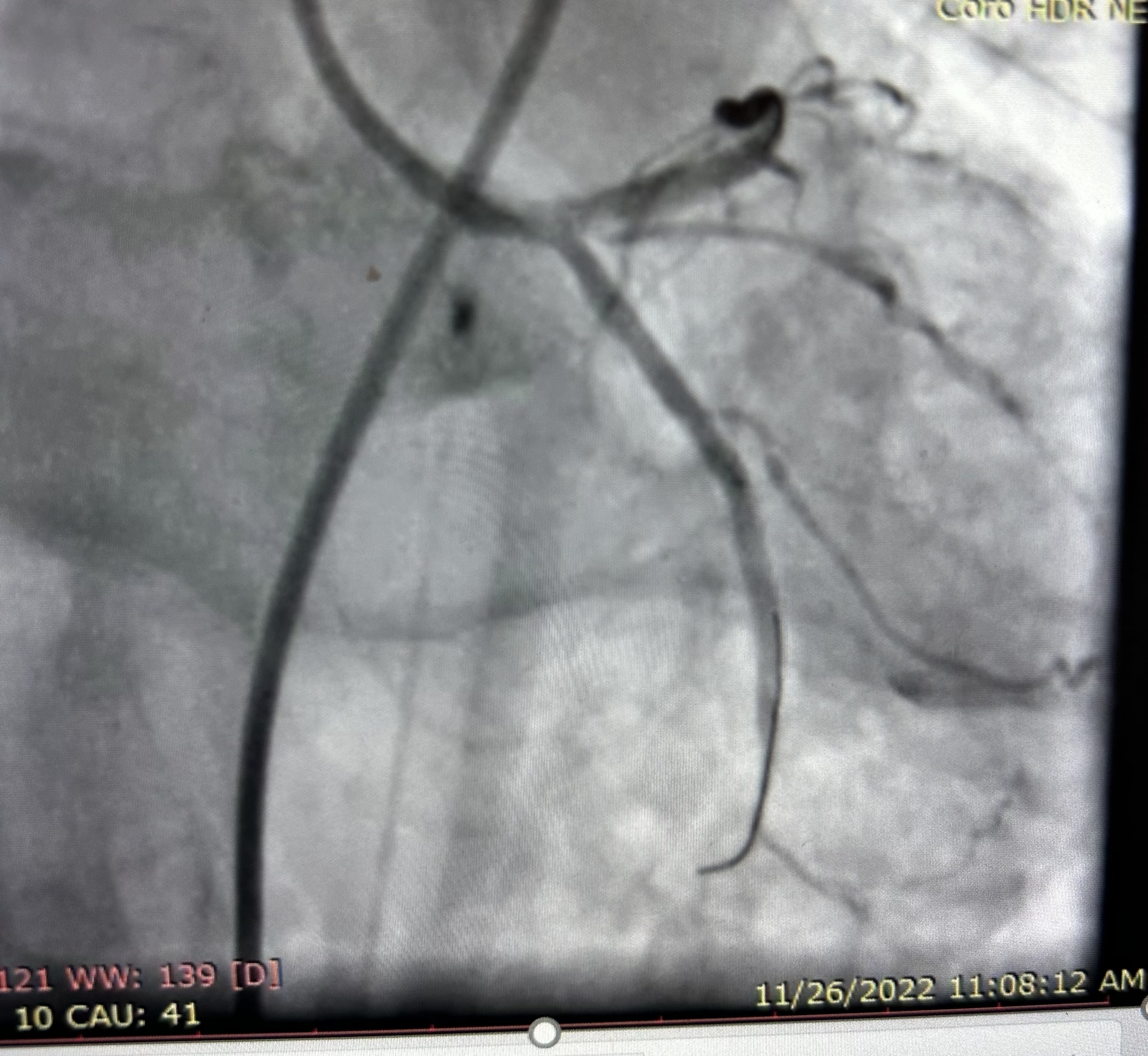
CAG REVEALED Left Main 50% with Calcified triple vessel disease


Interventional Management
Procedural Step
Heart team meeting was done,High risk for CABGso planned for PTCA/Stent to Left Main bifurcation stenting with Rotablation under IVUS guidanceRotablation to LAD/LCX done using 1.5mm Burr followed by NC balloonMini crush technique for bifurcation stenting used -2.75x24mm DES from Lt main to LCX and 3.5x24mm DES from Left main to LAD deplyoed followed by kissing balloon and POT by using 4,5mm balloon in Left Main.Final IVUS run taken with MSA of 6.1mm2 ,7.2 and 9.4mm2 in LCX/LAD and Left Main respectively
Case Summary
In hospital course
•2hrs later , patient had sudden hypotension, nausea,, vomiting, hematemesis
•Urgentendoscopy – large Mallory Weiss tear , hemoclipping done
•Antiplateletwithheld ,Hb dropped to 5 gm/dl, 3 PRBC Transfusion done
•SAPTstarted after 48hrs
•4th day -AF With FVR , medical cardioversiondone
•AcuteRT Lower limb DVT , Anticoagulation started
•Patientdischarged on day 7 on SAPT WITH NOAC
Conclusion:
•Bleedingand bleeding-related hospitalization are common in patients receiving DAPTafter PCI. In studies evaluating bleeding and thrombotic risk in patientstreated with DAPT after coronary stenting, clinically relevant bleedingoccurred in up to 6.2% of patients and up to 4.8% patients had bleeding-relatedhospitalization.The mostcommon site is Gastrointestinal bleeding.
•PatientsundergoingLM PCI , those with HBR are at increased risk of all cause death,MI MI and bleeding(4 fold)
•Frailtyand comorbidities are primary cause of worse outcomes in patient at HBR.
•Useof intracoronary imaging, trans-radial route, optimal selection of antiplateletstrategy has been shown to improve outcomes in these patients
•Multidisciplinaryapproach and team work helps in saving lives in these high risk patients

