Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-112
From Stalled to Flowing
By Iskandar Mirza Amran, Hafidz Abd Hadi, Kumara Gurupparan Ganesan, Shaiful Azmi Yahaya
Presenter
Iskandar Mirza Amran
Authors
Iskandar Mirza Amran1, Hafidz Abd Hadi1, Kumara Gurupparan Ganesan1, Shaiful Azmi Yahaya1
Affiliation
National Heart Institute, Malaysia1,
View Study Report
TCTAP C-112
Coronary - Complication Management
From Stalled to Flowing
Iskandar Mirza Amran1, Hafidz Abd Hadi1, Kumara Gurupparan Ganesan1, Shaiful Azmi Yahaya1
National Heart Institute, Malaysia1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 64 years old female patient presenting with a medical history of diabetes mellitus, hypertension, chronic kidney disease and hypothyroidism was referred to our center for non-ST elevation myocardia infarction.
Relevant Test Results Prior to Catheterization
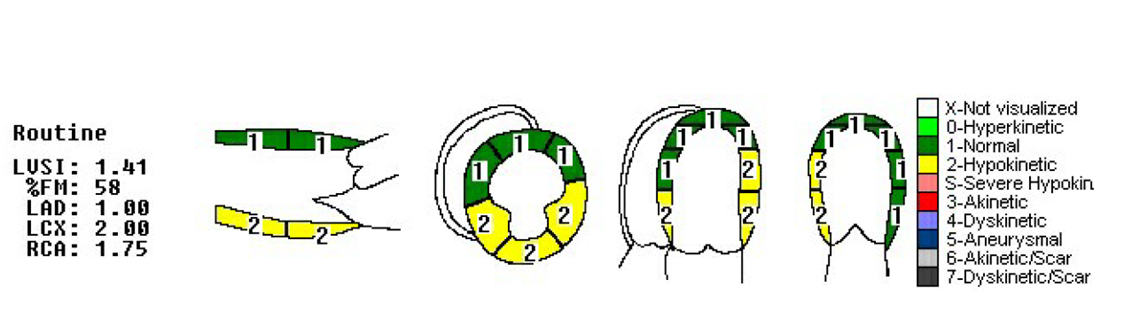
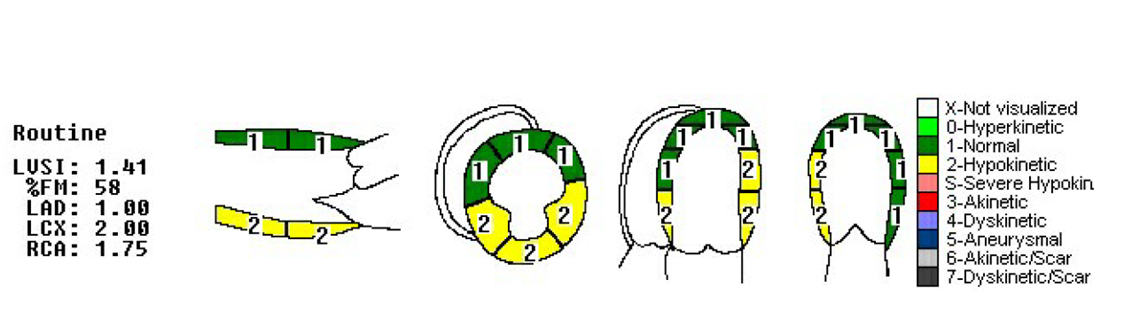
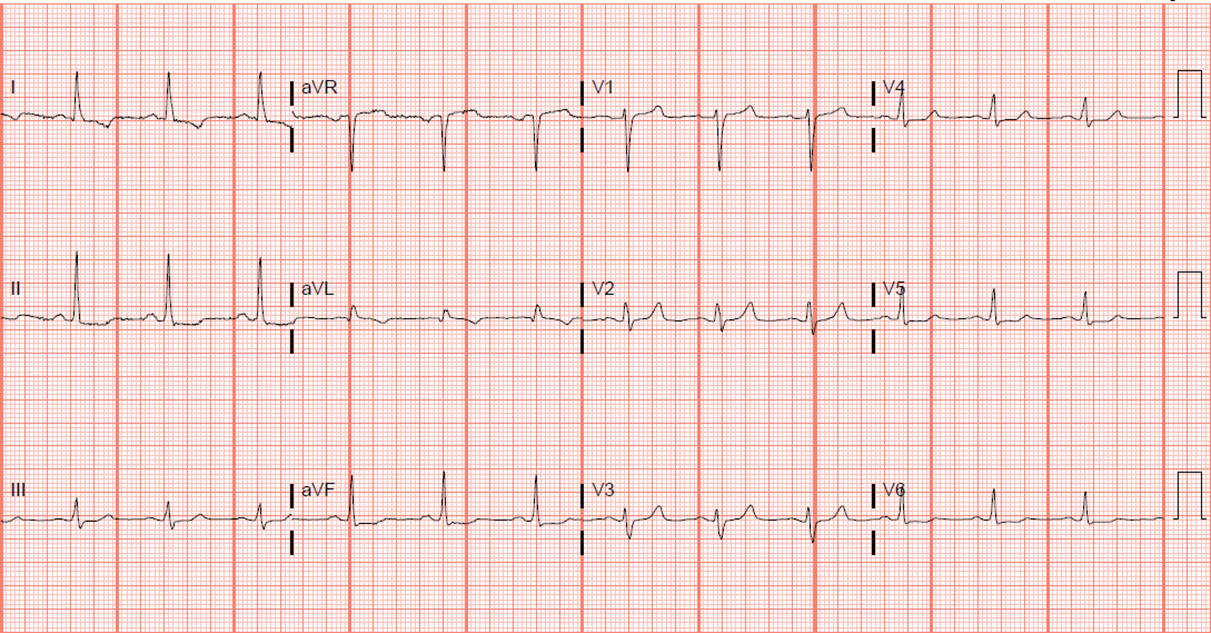
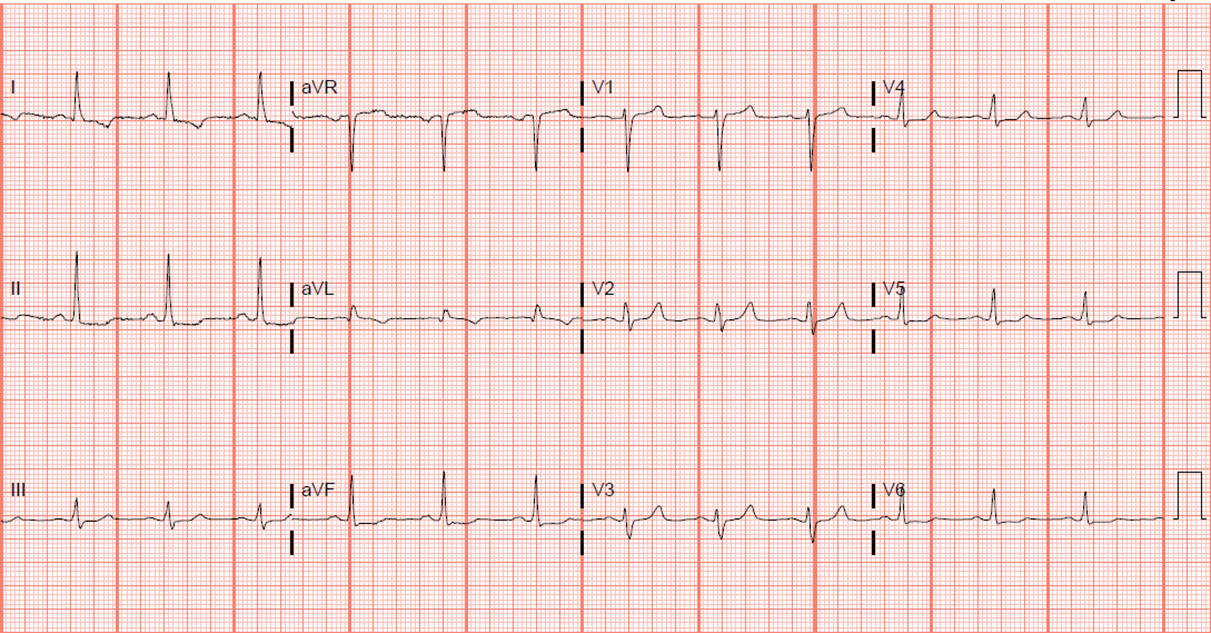
The electrocardiogram revealed 1 mm ST depression over lead 1,aVL and V5-6. Bloods investigations showed elevated fasting blood sugar levels of 18.2 mmol/L, troponin levels of 1040 and NT pro-BNP level of 7427. The echocardiogram indicated an ejection fraction of 49% and hypokinesia over the right coronary artery territory.
Relevant Catheterization Findings
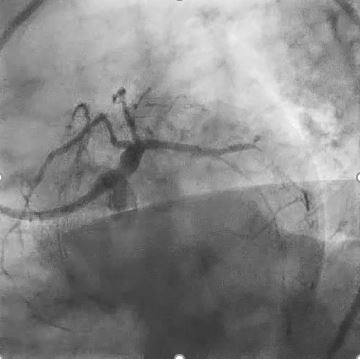
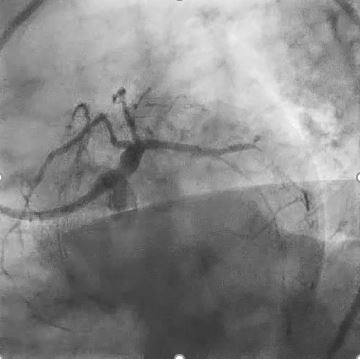
Diagnostic coronary angiography revealed severe three vessel disease, with significant proximal left anterior descending(LAD) artery disease, diffused mid-segment left circumflex(LCx) artery disease, and severe disease over the proximal and distal right coronary artery(RCA). Although patient was referred for coronary artery bypass graft surgery, she expressed reluctance towards it.




Interventional Management
Procedural Step
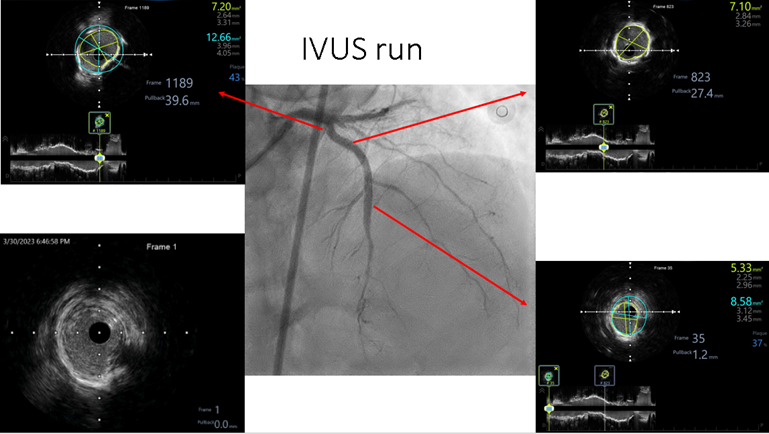
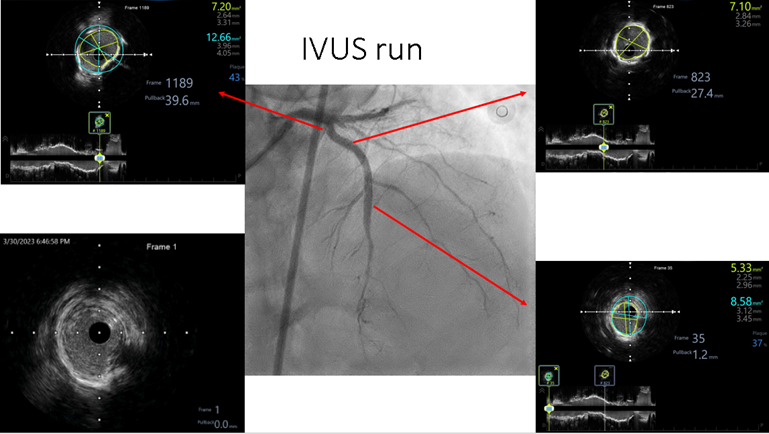
Consequently, we proceed with PCI on the RCA, successfully performing a drug-coated balloon procedure on the distal RCA and deploying 2 drug eluting stents at the mid and proximal sections, near the ostial RCA. Regarding LAD artery, Intravascular ultrasound (IVUS) showed MLA of 1.76 mm2 and 360 degree calcification with length of 8 mm. Lesion was pre-dilated using scoring balloon (2.75x10 mm), unfortunately cine showed no reflow post pre-dilatation. Patient developed hypotension and lesion pre-dilated again using non-compliant balloon (2.0x15mm), but the no-reflow phenomenon persist. At this point, we identified two potential causes: coronary artery dissection or distal thromboembolism. We stented the proximal LAD using DES (2.75x38 mm), however no reflow still persist. The patient condition deteriorated, leading to worsening hypotension and ventricular tachycardia, which required cardioversion twice to restore sinus rhythm. Thrombuster run was done for 3 cycle, yet no reflow phenomenon persisted. Ultimately, intracoronary bolus of adenosine was delivered using a thrombuster catheter, resulting in TIMI 3 flow restoration. The stent was post-dilated using a non-compliant balloon (3.0x15 mm), and IVUS imaging post stenting revealed a minimal stent area of 7.10 mm2, satisfactory stent apposition and no stent edge dissection.




Case Summary
In conclusion, the prevention and treatment of coronary reflow are of paramount importance, as the full benefits of reperfusion are only realized when coronary flow returns to normal. No reflow is associated with larger infarct size, reduced ejection fraction, and higher mortality rates. Pharmacological interventions have demonstrated efficacy and can be repeated as necessary. Preferably, distal intracoronary infusion via an infusion catheter should be employed to avoid systemic hemodynamic effects, rather than injection through the guiding catheter.

