Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-059
Long Term Clinical Outcome After Myocardial Revascularization for Multivessel Coronary Disease in Patients With Left Ventricular Dysfunction
By Hansu Park, Hoyun Kim, Jinho Lee, Yeonwoo Choi, Do-Yoon Kang, Jung-Min Ahn, Seung-Jung Park, Duk-Woo Park
Presenter
Hansu Park
Authors
Hansu Park1, Hoyun Kim2, Jinho Lee3, Yeonwoo Choi4, Do-Yoon Kang1, Jung-Min Ahn1, Seung-Jung Park1, Duk-Woo Park1
Affiliation
Asan Medical Center, Korea (Republic of)1, Bucheon Sejong Hospital, Korea (Republic of)2, Kyung Hee University Medical Center, Korea (Republic of)3, Changwon Hanmaeum Hospital, Korea (Republic of)4
View Study Report
TCTAP A-059
Multi-Vessel Disease
Long Term Clinical Outcome After Myocardial Revascularization for Multivessel Coronary Disease in Patients With Left Ventricular Dysfunction
Hansu Park1, Hoyun Kim2, Jinho Lee3, Yeonwoo Choi4, Do-Yoon Kang1, Jung-Min Ahn1, Seung-Jung Park1, Duk-Woo Park1
Asan Medical Center, Korea (Republic of)1, Bucheon Sejong Hospital, Korea (Republic of)2, Kyung Hee University Medical Center, Korea (Republic of)3, Changwon Hanmaeum Hospital, Korea (Republic of)4
Background
Long-termcomparative data on clinical outcomes between percutaneous coronaryintervention (PCI) and coronary artery bypass grafting (CABG) according to leftventricular (LV) function are limited.
Methods
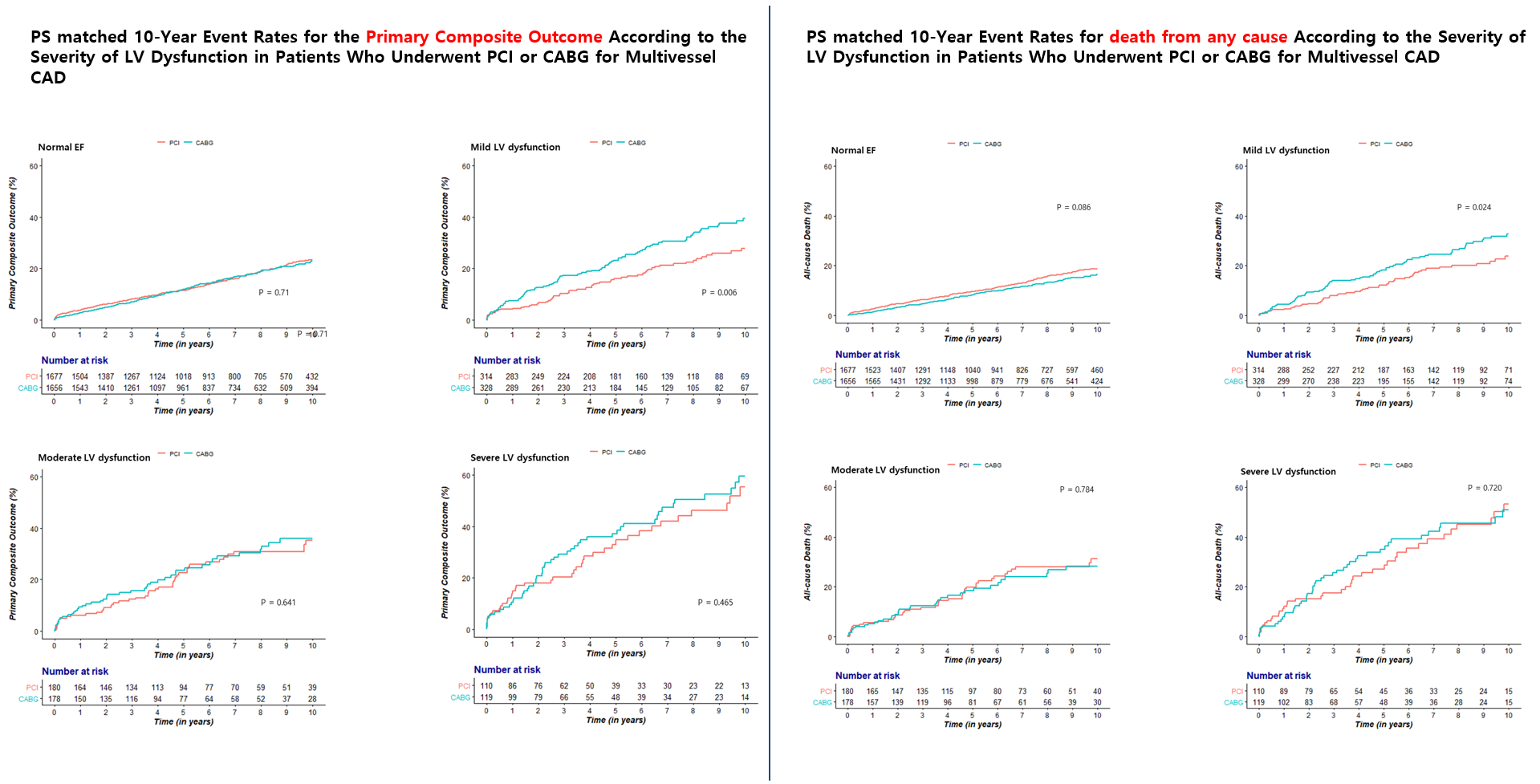
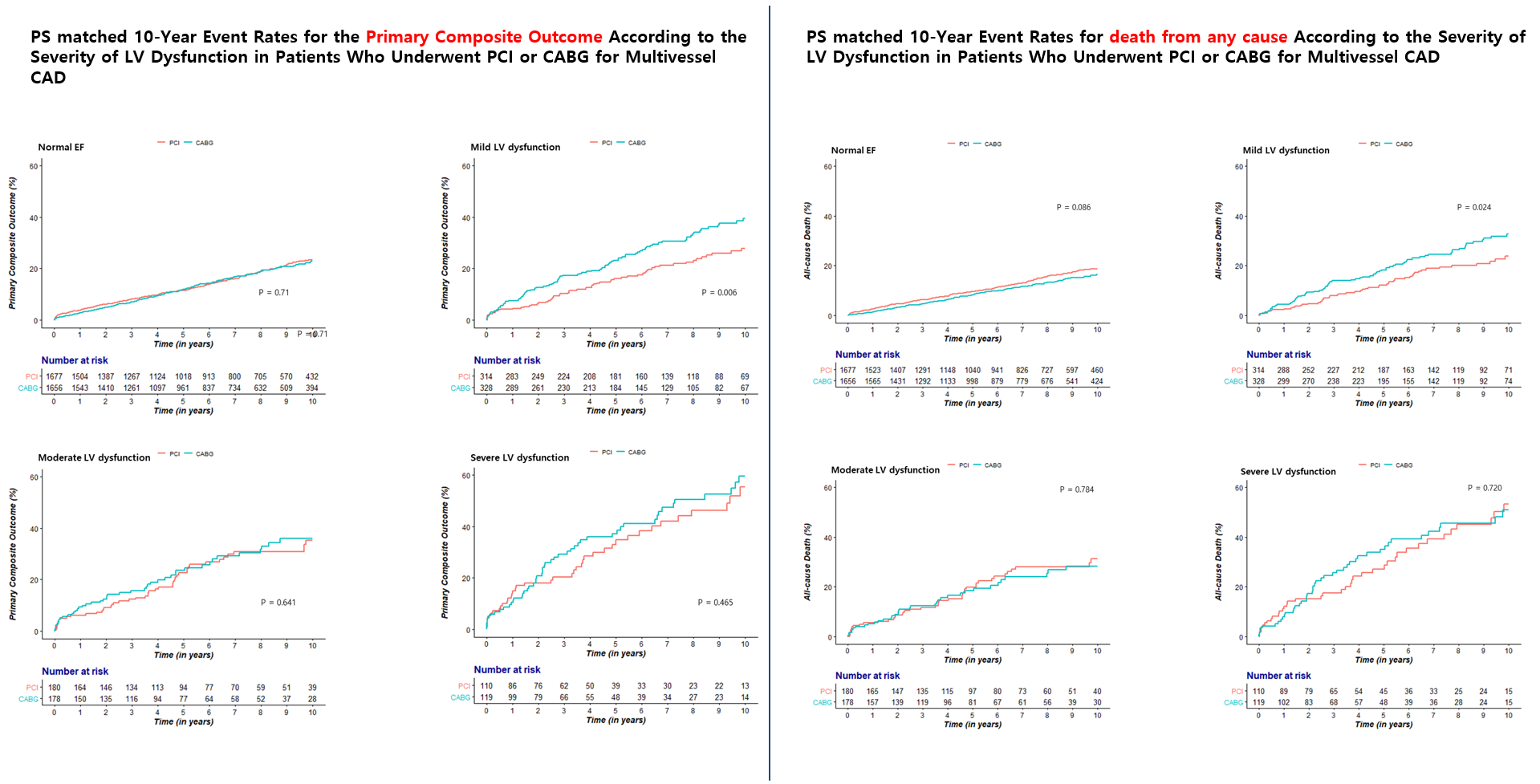
: From theAsan-Multivessel registry, we identified 9,856 patients who underwent CABG(n=4,107) or PCI (n=5,749). LV function was categorized according to LVEF asnormal function (LVEF ≥55%),mild (LVEF ≥45% to <55%),moderate (LVEF ≥35% to <45%), or severe (LVEF<35%) dysfunction. The primary composite outcome was a composite of death,spontaneous myocardial infarction, or stroke at 10 years. To adjust differencesof baseline risk factors, propensity-score matching and inverse probability of treatment weighting (IPTW) were used.
Results
Among 9,856 eligible patients, 7350 (74.5%) patients had normal LVEF and 1288 (13.0%), 715(7.2%), and 503 (5.1%) had mild, moderate, and severe LV dysfunction atbaseline, respectively. After propensity matching, PCI, as compared with CABG,had similar risks for the primary composite outcome in patients with normalLVEF (adjusted hazard ratio [HR] 0.97; 95% confidence interval [CI] 0.82−1.15; P=0.71), moderate LVEF (HR 1.10; 95% CI 0.74−1.64; P=0.641), or severe LVEF (HR 1.17; 95% CI 0.77−1.77;P=0.465). In patients with mild LVEF, PCI had a higher risk of primary outcomecompared to CABG (HR 1.15; 95% CI 1.13−2.13; P=0.006) (Figure and Table1). Afteradjustment using IPTW, however, the risk of the primary composite outcome wasnot significantly different between PCI and CABG according to LVEF (Table2).




Conclusion
In patients withmultivessel disease following myocardial revascularization, there were nosignificant differences in the primary composite outcome of death, MI, orstroke at 10 years between PCI and CABG according to left ventricular function.

