Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-007
Diagnostic Accuracy of Platelet to Lymphocyte Ratio for Predicting No Slow Reflow After Primary Percutaneous Coronary Intervention in Acute Myocardial Infarction: A Systematic Review and Meta-Analysis
By Hendy Bhaskara Perdana Putra, Intan Dwistya Wiraguna, Noer Halimatus Syakdiyah, Libriansyah -, Richardus Rukma Juslim
Presenter
Hendy Bhaskara Perdana Putra
Authors
Hendy Bhaskara Perdana Putra1, Intan Dwistya Wiraguna2, Noer Halimatus Syakdiyah3, Libriansyah -1, Richardus Rukma Juslim1
Affiliation
Dr. Ramelan Navy Hospital Surabaya, Indonesia1, RS Universitas Airlangga, Indonesia2, Airlangga University, Indonesia3
View Study Report
TCTAP A-007
ACS/AMI
Diagnostic Accuracy of Platelet to Lymphocyte Ratio for Predicting No Slow Reflow After Primary Percutaneous Coronary Intervention in Acute Myocardial Infarction: A Systematic Review and Meta-Analysis
Hendy Bhaskara Perdana Putra1, Intan Dwistya Wiraguna2, Noer Halimatus Syakdiyah3, Libriansyah -1, Richardus Rukma Juslim1
Dr. Ramelan Navy Hospital Surabaya, Indonesia1, RS Universitas Airlangga, Indonesia2, Airlangga University, Indonesia3
Background
Primary Percutaneous Coronary Intervention (PCI) continues to be the primary approach for reestablishing blood flow during acute myocardial infarction (MI). Despite the successful restoration of epicardial coronary artery patency following PCI, there is a risk of No Slow Reflow (NSR) phenomenon may not be entirely averted.Several studies have shown that Platelet to Lymphocyte Ratio (PLR) may predict incidence of NSR phenomenon and associate with mortality and adverse outcomes in PCI. We performed this systematic review and meta – analysis to obtain summary estimates of the diagnostic accuracy of PLR to predict NSR phenomenon in acute MI which treated with Primary PCI.
Methods
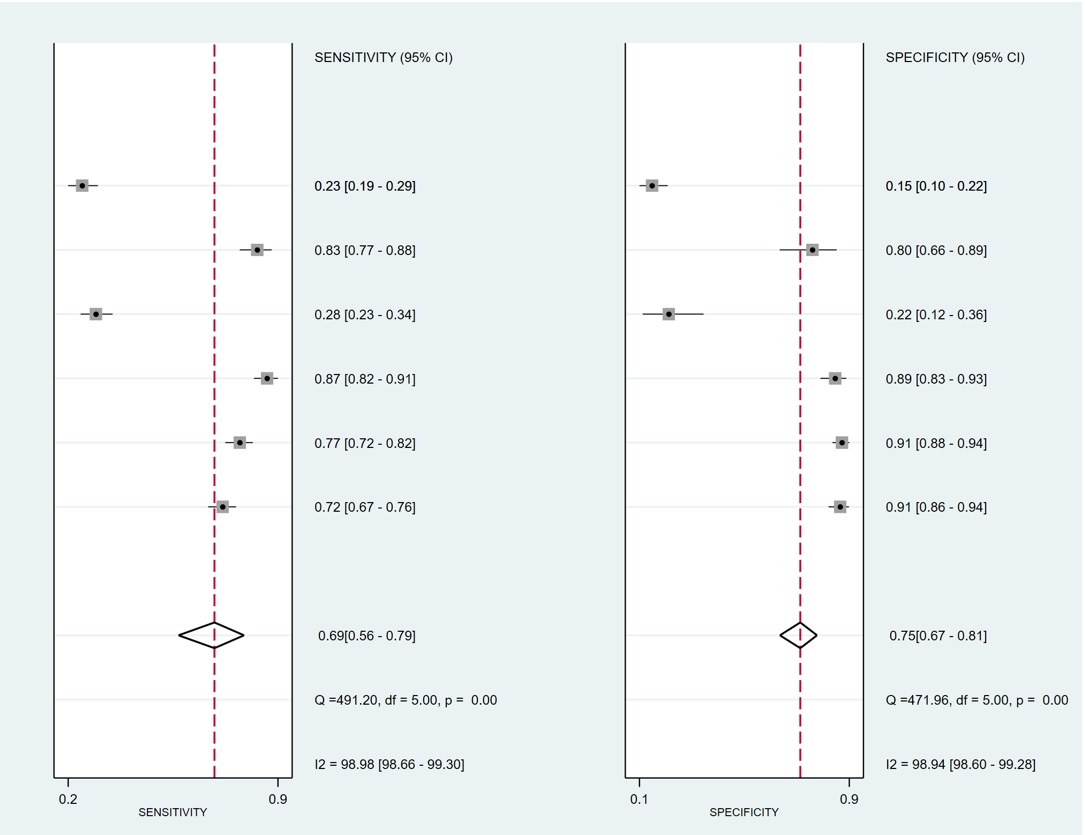
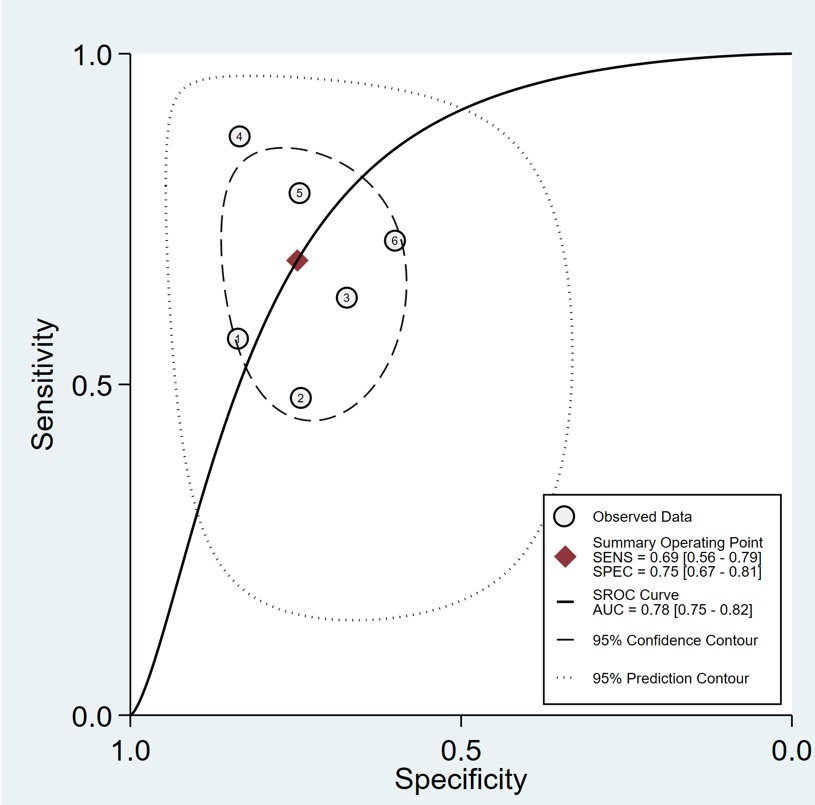
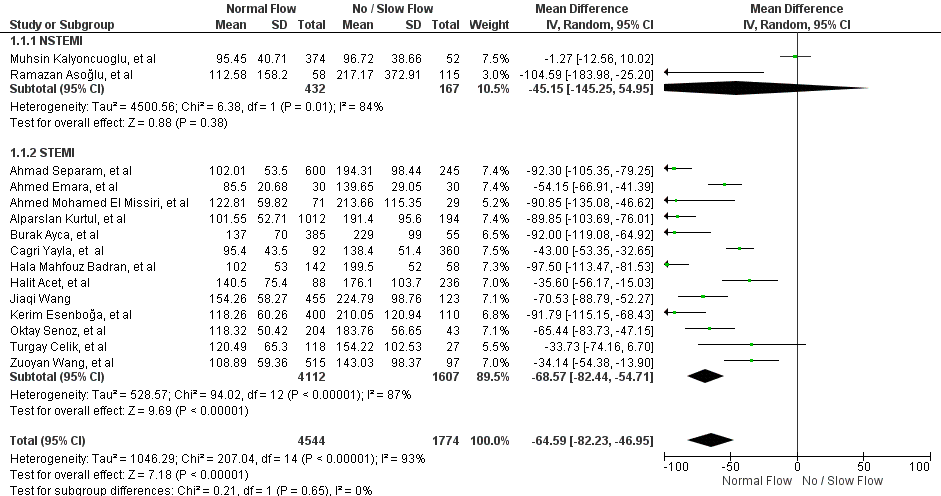
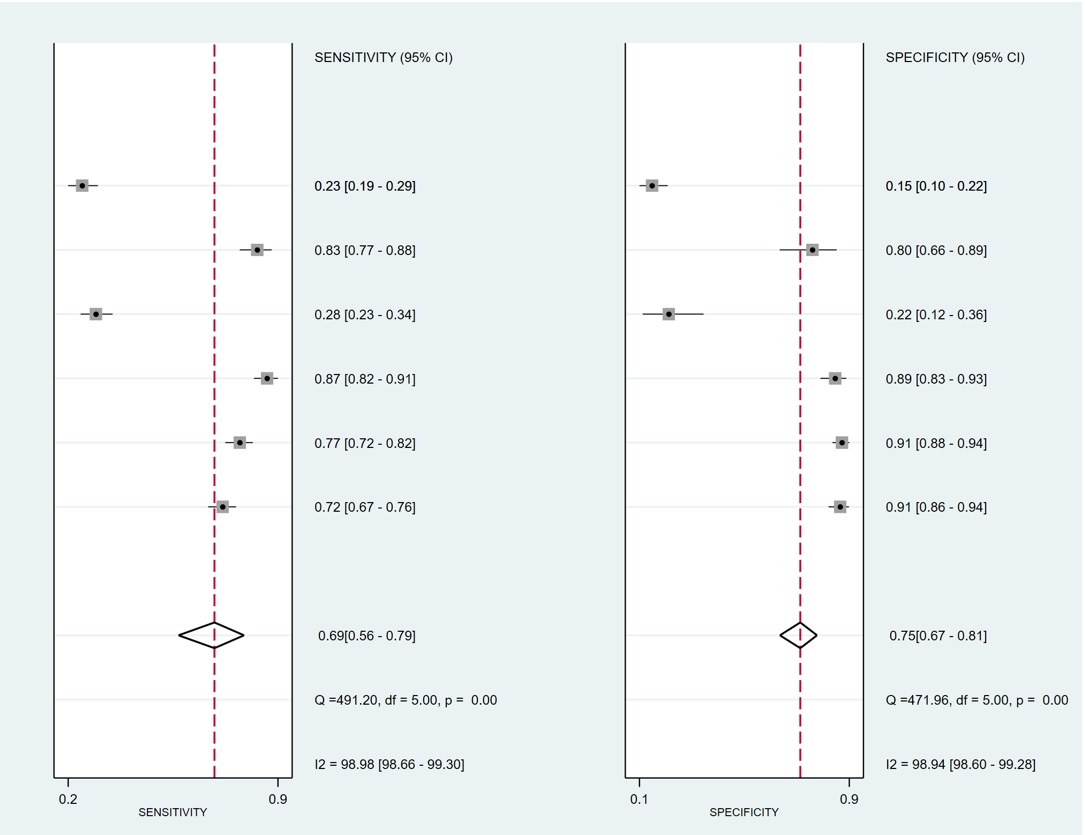
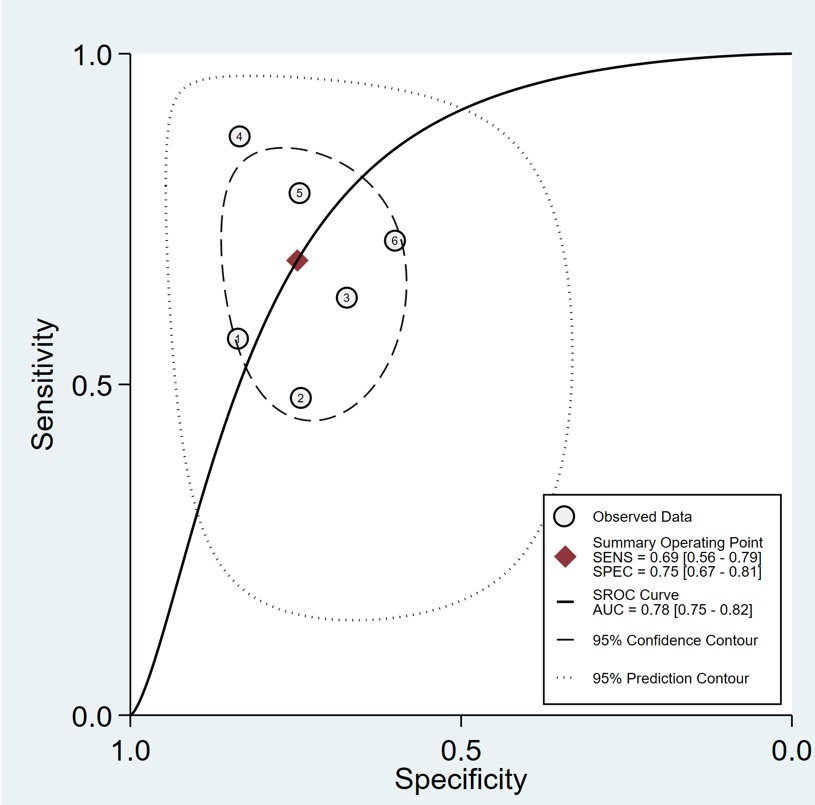
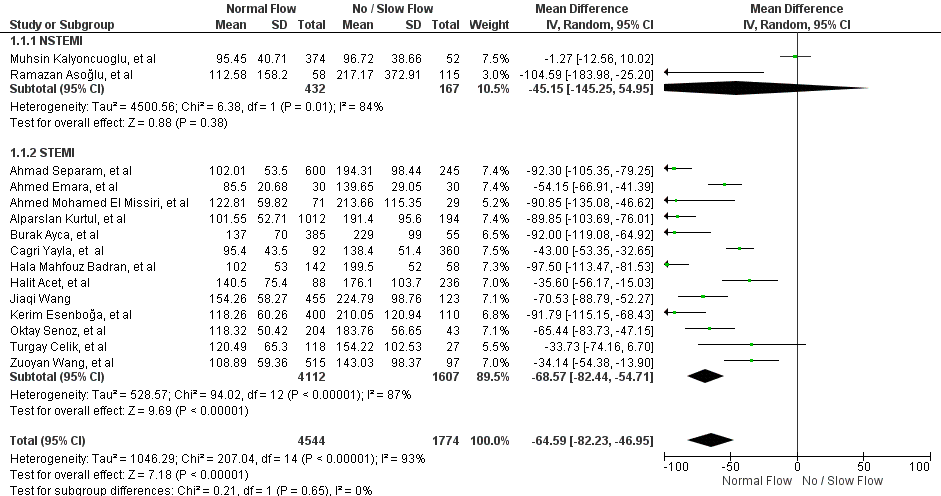
This study was conducted according to PRISMA – DTA statement. We performed a systematic literature search from several electronic databases. Criteria inclusion were Randomized Control Trial (RCT) or observational study which reported initial PLR in patients with acute MI who undergone Primary PCI and developed NSR phenomenon. Primary outcome were summary points (pooled sensitivity and specificity, positive likelihood ratio, negative likelihood ratio, diagnostic odds ratio), and summary lines (SROC curve). Furthermore, we also assess mean difference (MD), with 95% confidence intervals (CIs) between no NSR phenomenon and NSR phenomenon group, as a secondary outcome.
Results
Fifteen studies were selected with 6.318 patients met the inclusion criteria and were included. However only six studies had their data processed into summary points and summary lines. The pooled sensitivity of PLR for predicting NSR phenomenon in patients with acute MI who undergone Primary PCI was 0.69 (95% CI [0.56-0.79]), with specificity was 0.75 (95% CI [0.67-0.81]). The positive likelihood ratio was 2.7 (95% CI [1.9-3.9]), the negative likelihood ratio was 0.42 (95% CI [0.28-0.62]), diagnostic odds ratio was 7 (95% CI [3-13]). The area under the curve of the summary receiver operator characteristic (SROC) was 0.78 (95% CI [0.75-0.82]). The optimal cut off point was 190. Furthermore, patient with normal reflow have lower PLR level (MD= -64.59 [95% CI, -82.23;-46.95],p=0.03).
Conclusion
Patient who developed NSR after Primary PCI had higher level of PLR. And PLR might be able to play a more important role in predicting NSR phenomenon in patients with acute MI who undergone Primary PCI.

