Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-056
Study of Change in N-Terminal Pro-Brain Natriuretic Peptide Levels in Patients Undergoing Percutaneous Balloon Mitral Valvuloplasty and Correlation With Echocardiographic and Hemodynamic Parameters
By Suresh Kumar Paidi
Presenter
Suresh Kumar Paidi
Authors
Suresh Kumar Paidi1
Affiliation
NRI Institute of Medical Sciences, India1
View Study Report
TCTAP A-056
Other Structural Interventions
Study of Change in N-Terminal Pro-Brain Natriuretic Peptide Levels in Patients Undergoing Percutaneous Balloon Mitral Valvuloplasty and Correlation With Echocardiographic and Hemodynamic Parameters
Suresh Kumar Paidi1
NRI Institute of Medical Sciences, India1
Background
The change in serum levels of NT-proBNP (N-terminal pro-brain natriuretic peptide) is considered as reflection of hemodynamic alterations. The decrease in pressures in the left atrium (LA) and right side of the heart following PBMV cause a decrease in wall stress which contributes to the decreased NT-proBNP levels. Present study is designed to assess the change in serum levels of NT-proBNP following PBMV (percutaneous balloon mitral valvuloplasty) and association between NT-proBNP reduction and various echocardiographic and hemodynamic parameters.
Methods
This is a Prospective Observational study consisted of 92 patients with rheumatic severe mitral stenosis (MS) who underwent PBMV. Serum NT-proBNP levels were measured 30minutes prior to the commencement of PBMV and 24 hours after PBMV. These values were correlated with various echocardiographic and hemodynamic parameters which were obtained before and after procedure.
Results
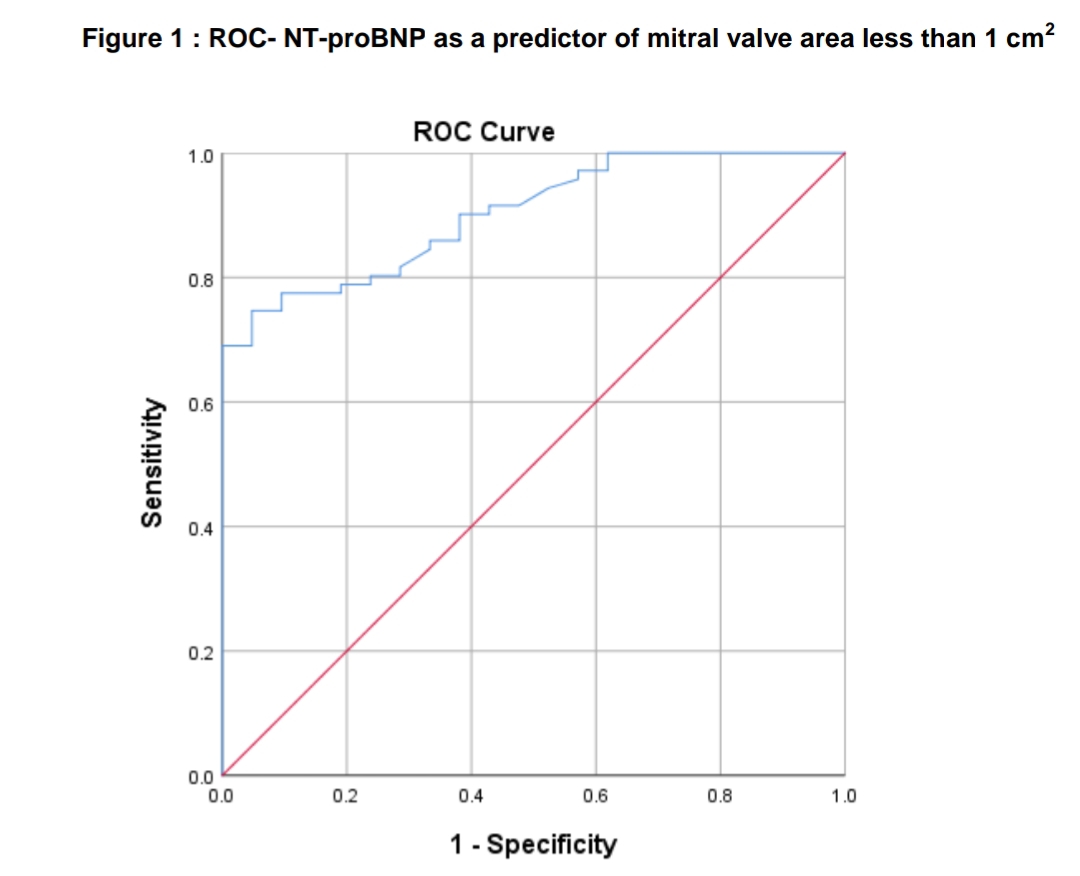
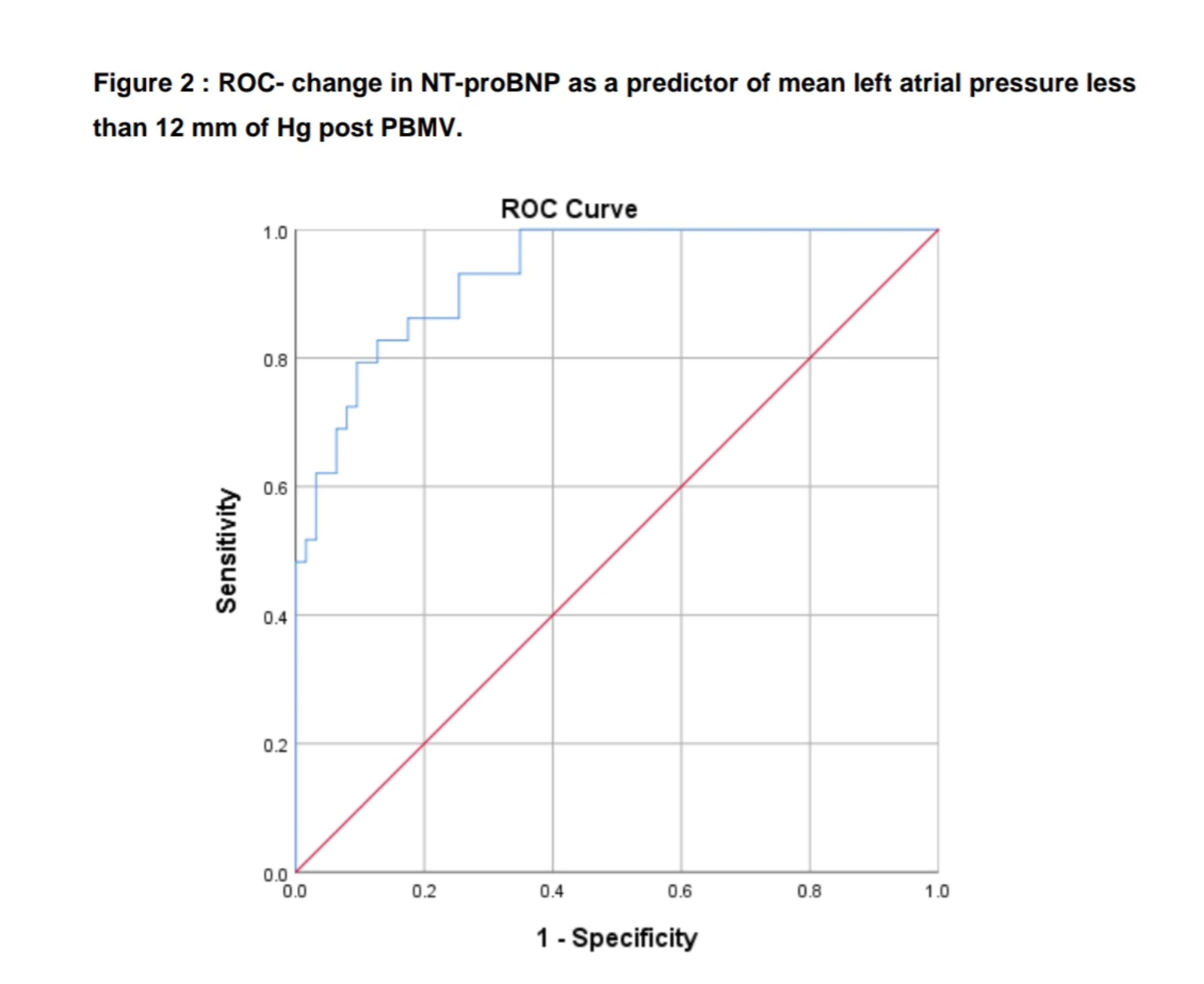
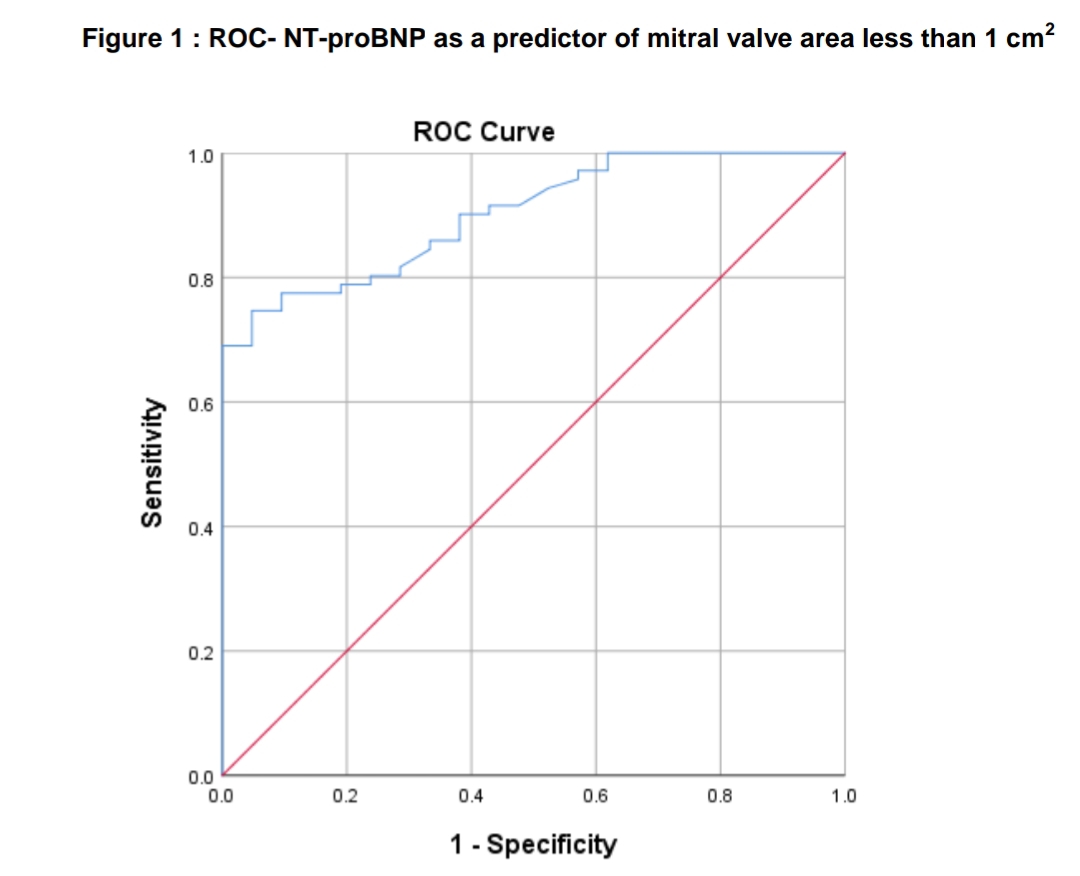
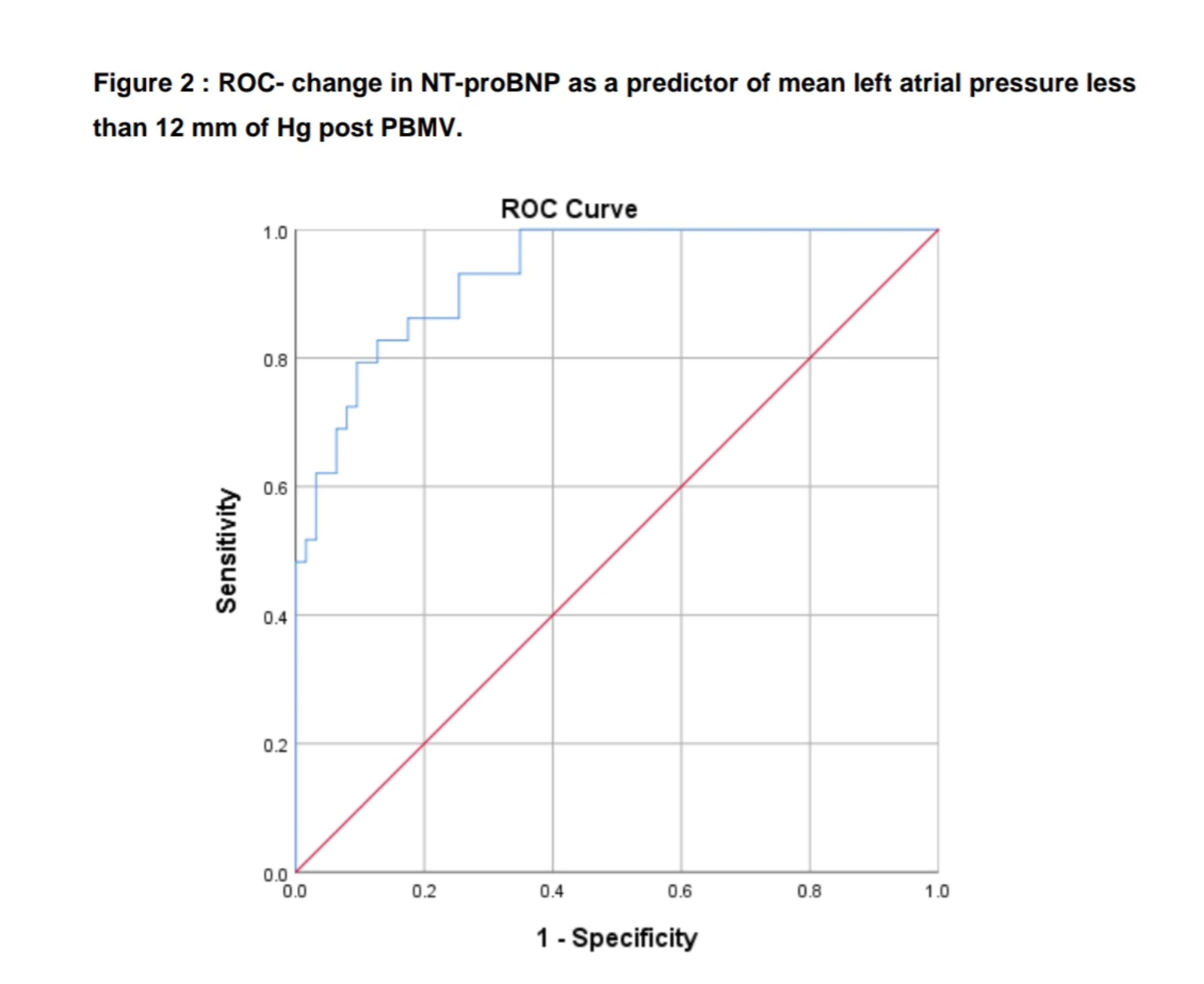
Eighty percent of the study population were women, and the common presenting symptom was dyspnea which was present in 100% of the patients. Baseline NT-proBNP levels in these patients significantly correlated with New York heart association (NYHA) functional class (r = 0.377; p < 0.001), left atrial diameter (r = 0.207; p 0.047), mean pulmonary artery pressures (r = 0.338; p < 0.001) and mean left atrial pressures (r = 0.207; p 0.048). Patients in atrial fibrillation had significantly higher NT-proBNP levels than patients in sinus rhythm (775 vs 481; p <0.001). All patients who underwent successful PBMV showed a significant decrease in NT-proBNP (decreased from a mean 580 pg/mL to 328 pg/mL) along with a significant improvement in various echocardiographic and hemodynamic parameters (p < 0.001). The change in NT-proBNP correlated significantly with the improvement with mean left atrial pressure (r = 0.407; p 0.020). Area under the ROC for NT-proBNP as a predictor of mitral valve area less than 1 cm2 was 0.90 [95% CI 0.84-0.96]. When using a NT-proBNP cut-off value of more than 302 pg/ml, sensitivity was 90.1% and specificity was 61.9%. Area under ROC for change in NT-proBNP post PBMV as a predictor of mean left atrial pressure less than 12 mm of Hg post PBMV was 0.93 [95% CI 0.88-0.98], when using change in NT-proBNP post PBMV, cut-off value of more than 238.5 pg/ml, sensitivity of 93.1% and specificity of 74.6%.
Conclusion
The decrease in serum NT-proBNP levels post procedure reflects procedural success as evidenced by correlation between reduction in NT-proBNP and improvement in echocardiographic and hemodynamic parameters, hence it is reasonable to consider serum NT-proBNP as a marker of successful PBMV.

