Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-018
The Utilization of Quantitative Flow Ratio (QFR) Study for Decision in Percutaneous Coronary Intervention and Outcomes
By Samshol Sukahri, Imran Zainal Abidin, Wan Azman Wan Ahmad, Ahmad Syadi Mahmood Zuhdi, Kok Han Chee, Ramesh Singh Argan Singh, Alexander Loch, Nor Ashikin Md Sari, Syuhada Khairul Anuar, Kee Wei Lee, Muhammad Azlan Aseri, Mohamad Rodi Isa
Presenter
Samshol Sukahri
Authors
Samshol Sukahri1, Imran Zainal Abidin2, Wan Azman Wan Ahmad2, Ahmad Syadi Mahmood Zuhdi2, Kok Han Chee2, Ramesh Singh Argan Singh2, Alexander Loch2, Nor Ashikin Md Sari2, Syuhada Khairul Anuar2, Kee Wei Lee2, Muhammad Azlan Aseri3, Mohamad Rodi Isa4
Affiliation
Kedah Medical Centre, Malaysia1, University Malaya Medical Centre, Malaysia2, University Malaya Medical Center, Malaysia3, Universiti Teknologi MARA, Malaysia4
View Study Report
TCTAP A-018
Angiography/QCA
The Utilization of Quantitative Flow Ratio (QFR) Study for Decision in Percutaneous Coronary Intervention and Outcomes
Samshol Sukahri1, Imran Zainal Abidin2, Wan Azman Wan Ahmad2, Ahmad Syadi Mahmood Zuhdi2, Kok Han Chee2, Ramesh Singh Argan Singh2, Alexander Loch2, Nor Ashikin Md Sari2, Syuhada Khairul Anuar2, Kee Wei Lee2, Muhammad Azlan Aseri3, Mohamad Rodi Isa4
Kedah Medical Centre, Malaysia1, University Malaya Medical Centre, Malaysia2, University Malaya Medical Center, Malaysia3, Universiti Teknologi MARA, Malaysia4
Background
Functional evaluation is crucial for diagnosing undetermined coronary artery stenosis in stable coronary artery disease. Fractional flow reserve (FFR) serves as the gold standard for assessing the physiological severity of coronary stenosis. Several trials have revealed a reverse correlation between post-interventional FFR and the risk of adverse events. Many studies endorse FFR-guided interventions, and current guidelines recommend FFR assessment for obstructed-mediated ischemia. However, FFR-guidance has its limitations, such as the requirement for drug-induced hyperemia (typically adenosine), patient discomfort, prolonged procedure time, and reimbursement challenges. To address these limitations, various methods based on 3D imaging modalities have been developed to derive FFR without invasive pressure wires or hyperemic agents. One such 3D imaging modality is Quantitative Flow Ratio (QFR), a novel technique capable of rapidly computing FFR from coronary angiography. QFR demonstrates a strong correlation with FFR and has proven clinical value in guiding both pre- and post-percutaneous coronary intervention (PCI) management. This pilot study aims to evaluate the impact of QFR-guided interventions in influencing decision-making processes for angioplasty and post-intervention procedures within the cardiology unit at the University Malaya Medical Centre.
Methods
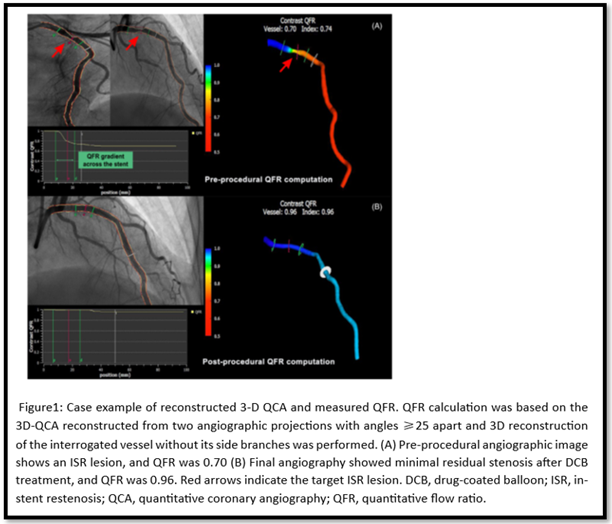
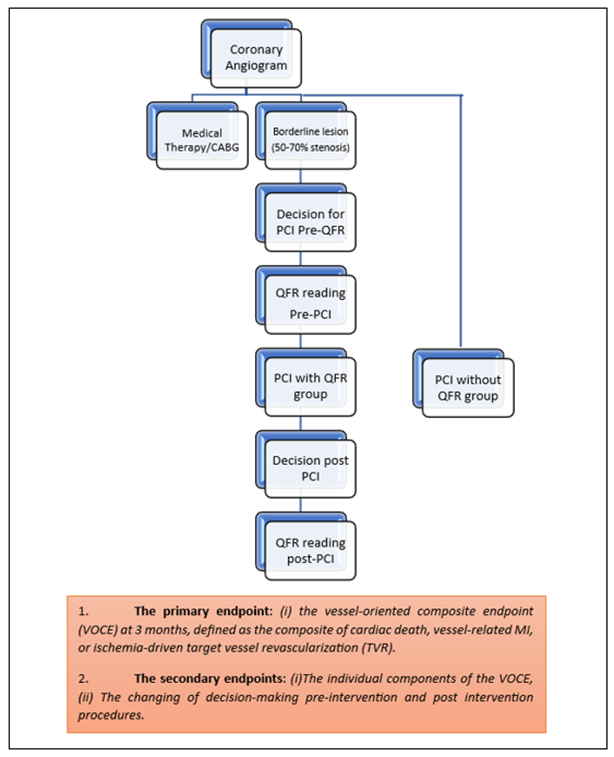
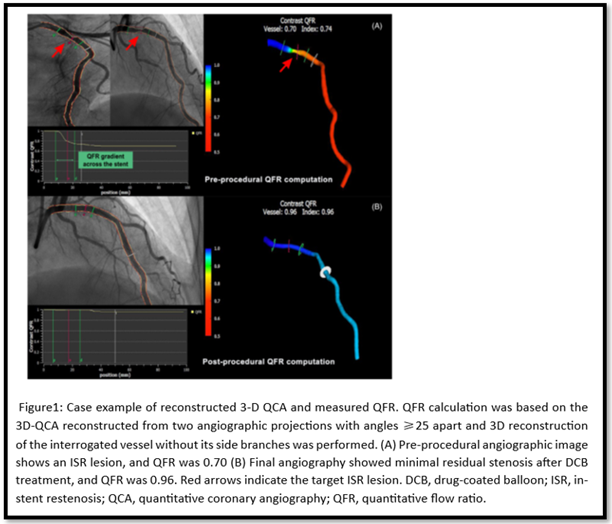
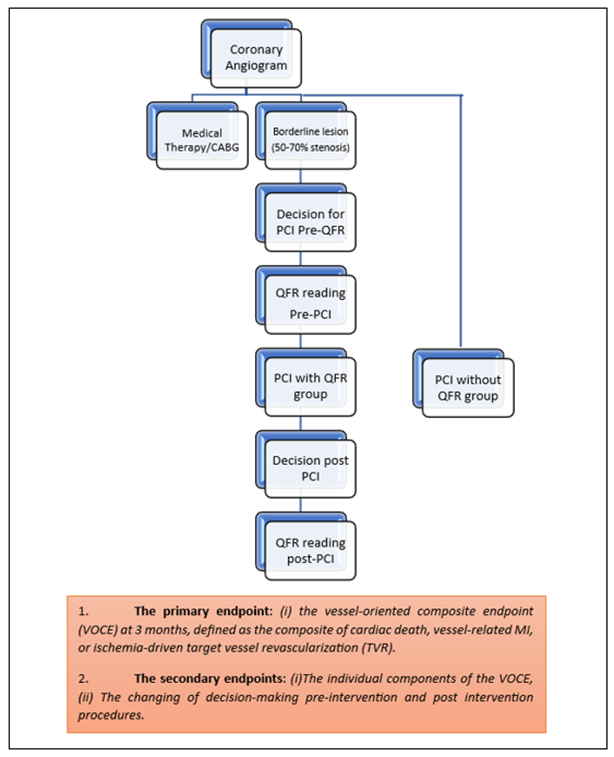
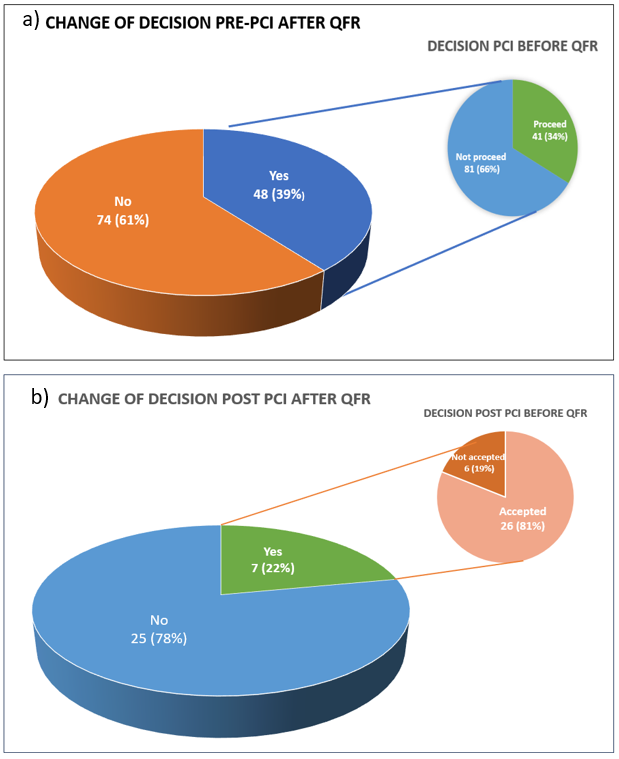
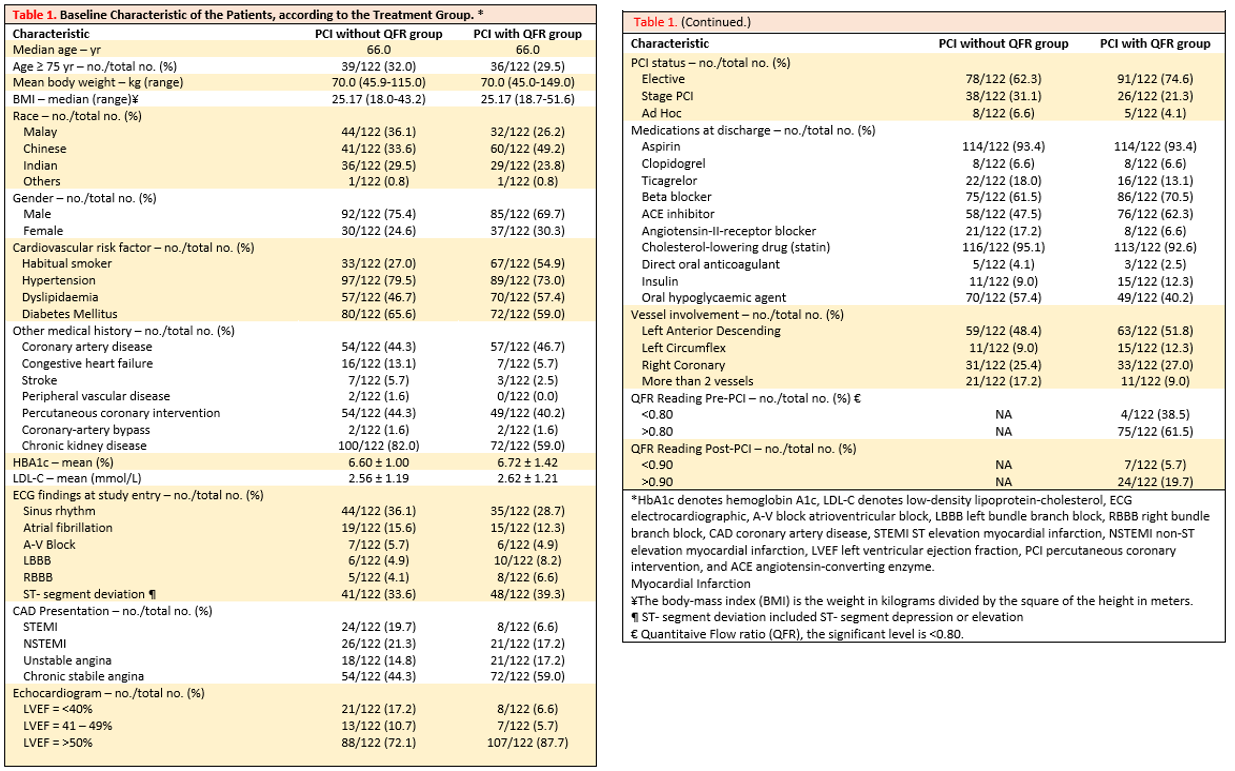
The pilot study conducted at UMMC from January 1, 2023, to July 31, 2023, involved all patients undergoing angiogram procedures. Patients were chosen based on specific inclusion and exclusion criteria (refer to Table 1). After the initial angiograms, the cardiologist determined the need for intervention. Subsequently, a Quantitative Flow Ratio (QFR) reading was obtained. Quantitative coronary angiography analyses were performed both before and after angioplasty using an offline computerized quantitative coronary angiographic system. Parameters measured included the reference vessel diameter (RVD), minimal lumen diameter (MLD), and percent diameter stenosis (%DS) (see Figure 1). If the QFR was >0.80, it was considered non-significant, and if <0.80, it indicated significant stenosis, leading to angioplasty. After angioplasty, the lesion was re-evaluated, and another QFR reading was taken. If the QFR was >0.90, no further intervention was required. The primary objective of the study is to collect and analyze data related to the decision-making process before and after QFR readings and post-angioplasty assessments. Outcomes will be assessed at discharge and during a 3-month follow-up for both the PCI with QFR group and the PCI without QFR group (refer to Figure 2). Statistical analysis will involve presenting continuous variables as medians with interquartile ranges. Group comparisons for PCI with QFR and PCI without QFR will be conducted using the Mann–Whitney U test for continuous variables. Categorical variables will be summarized using frequencies and proportions, and comparisons will be made using Pearson's chi-square or Fisher's exact test. It's worth noting that this study has received ethical approval from the UMMC Medical Research Ethics Committee (MREC).


Results
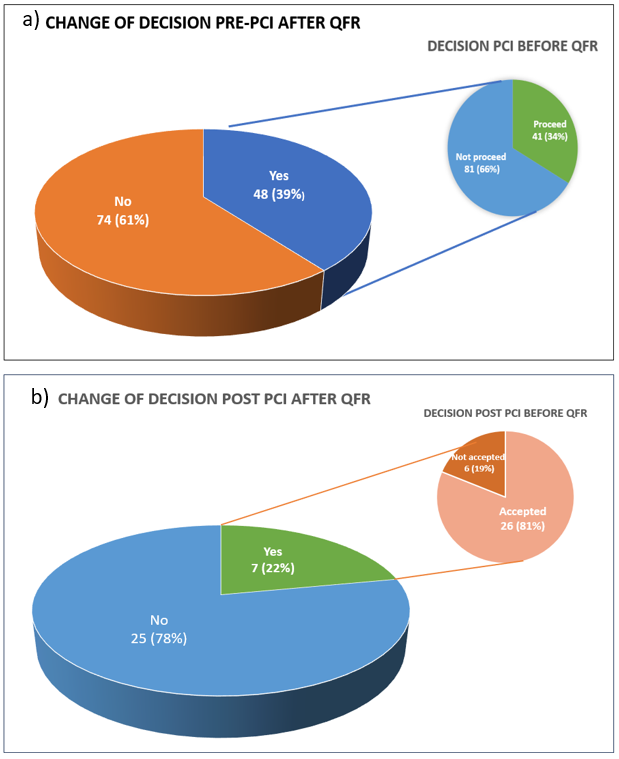
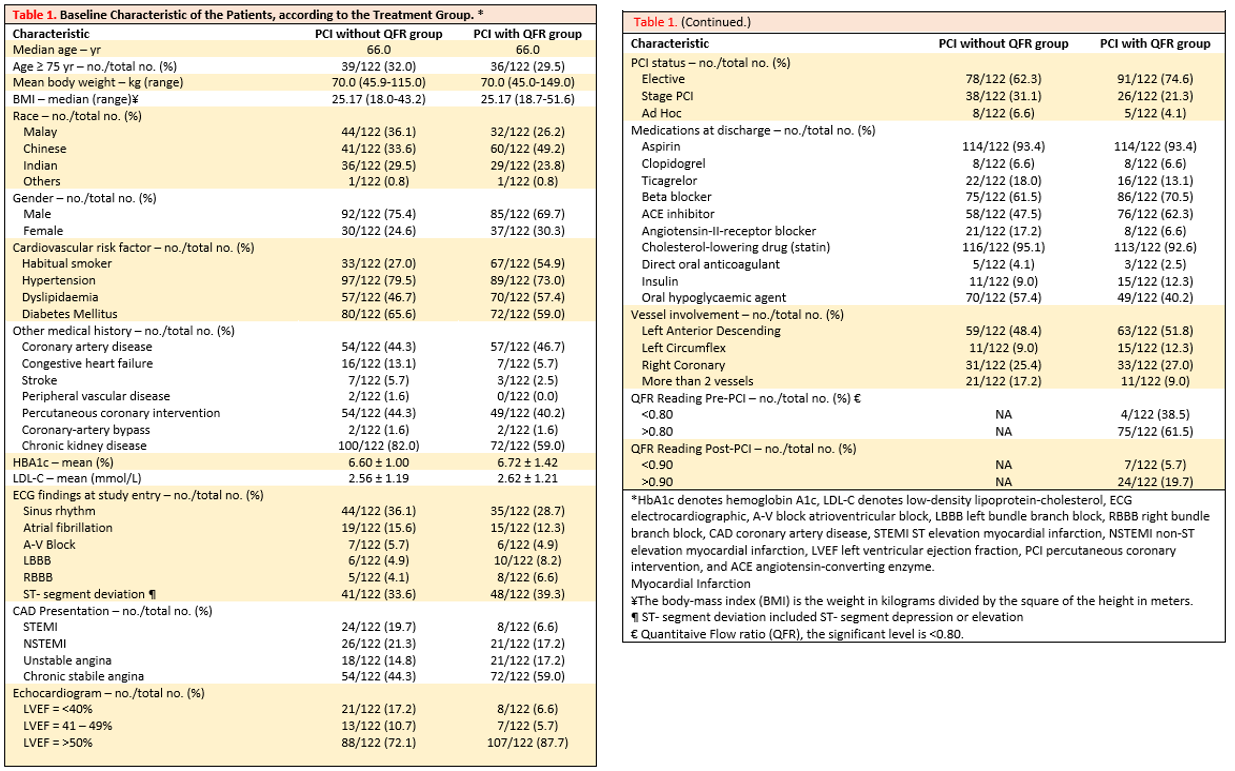
The Baseline characteristics revealed a median age of 66 for both groups, with similar body weight and BMI ranges (Table 2). Malays dominated the PCI without QFR group (36.1%), while Chinese were prevalent in the PCI with QFR group (49.2%). Males outnumbered females in both groups (75.4% vs. 69.7%). Most patients were non-smokers, with 27% in the PCI without QFR group and 54.9% in the PCI with QFR group. Hypertension was the primary cardiovascular risk factor, affecting 79.5% and 73% of patients in each group, followed by diabetes and dyslipidemia. Chronic kidney disease was prevalent (82% and 59%) in both groups. Glycemic control was similar, with mean HbA1c and LDL-C levels close in both groups. ECG findings indicated a predominance of normal sinus rhythm, followed by ST-segment deviation. Chronic stable angina was the most common coronary artery disease presentation, and most patients had preserved ejection fractions above 50%. Most procedures were elective, with aspirin and statin medications frequently prescribed at discharge. The left anterior descending artery (LAD) was the most frequently involved vessel in both groups. Regarding QFR readings, 61.5% of patients had a normal pre-PCI reading (>0.80), and 19.7% exhibited a normal QFR reading post-PCI. The primary objective, Vessel-oriented Composite Endpoint (VOCE) at the 3-month follow-up, showed one cardiac death in the PCI without QFR group and none in the PCI with QFR group (Table 3). However, this difference was not statistically significant (p = 0.316). Secondary endpoints examining individual components of VOCE indicated one cardiac death in the PCI without QFR group. In terms of decision-making, changes were more prevalent in pre-intervention assessments. Among the 122 subjects who underwent QFR measurements, 39% experienced decision changes. Specifically, 34% initially slated for angioplasty changed their decision to proceed, while 66% opted not to proceed. Post-PCI decision changes after QFR readings were less common (22%). Out of these, 19% chose not to accept the results and sought further intervention, while 81% accepted the results (Figure 3).


Conclusion
In conclusion, our study underscores the pivotal role of Quantitative Flow Ratio (QFR) measurements in the assessment of patients with borderline angiographic lesions (50-70% stenosis). QFR proves to be a valuable modality for evaluating coronary physiology, enabling informed decisions regarding angioplasty. Furthermore, the incorporation of QFR measurements post-PCI significantly bolsters confidence in concluding the procedure, offering a more comprehensive understanding of its success. However, it's imperative to acknowledge the limitations of our study. We encountered time constraints that limited the duration of follow-up for assessing outcomes. Additionally, the relatively small sample size, as well as the presence of selection bias due to non-randomized patient selection during the angiogram procedure, should be recognized as potential limitations. While our findings are indeed promising and provide valuable insights, it is essential to emphasize that further research is warranted. Future investigations should encompass larger and more diverse datasets, permitting longer-term follow-up to comprehensively evaluate the impact of QFR on the vessel-oriented composite outcome (VOCE). This continued research will help solidify the significance of QFR in clinical practice and its potential benefits for patients with borderline angiographic lesions.

