TCTAP A-015
ACS/AMI
Clinical Insights: Impact of BMI and Gender on Postoperative Myocardial Ischemia Following Remote Ischemic Preconditioning in Cardiac Surgery - A Meta-Regression Analysis
Ameer Fadhil Abbas Al Wssawi1, Armand Gumera2, Ahmed Ibrahim3, Hashim Talib Hashim4, Ali Saad Al-Shammari5, Ghadeer Mohammed Abbas6, Mohannad Gamal Abdeltawwab7, Mahmoud Amim8, Urooj Shamim9, Mohanad Alchamaley1
University of Al-Qadisiyah, Iraq1, University of Melbourne, Australia2, Alexandria University, Egypt3, University of Warith Al-Anbiyaa, Iraq4, Al-Kindy general hospital, Iraq5, University of Kufa, Iraq6, Fayoum University, Egypt7, Fayoum University Hospital, Egypt8, The Aga Khan University Hospital, Pakistan9
Background
Background: In cardiac surgery, patients are vulnerable to the serious complication of postoperative myocardial ischemia, which can be a detriment to patient outcomes. Whilst great strides have been made in minimizing perioperative risks through the development of improved anesthesia protocols and minimally invasive techniques, the challenge of postoperative myocardial ischemia continues as a contributor to mortality and extended hospital stays. Remote Ischemic Preconditioning (RIPC) has appeared as a promising procedural adjunct via the activation of endogenous defensive mechanisms to lessen ischemic injury. However, the efficacy of RIPC has been a recent topic of discussion, and the evidence for its association with patient-specific characteristics has been insufficient. The current literature has observed the effectiveness of RIPC in a varied patient population, without adequate analysis of how patient characteristics including Body Mass Index (BMI), gender, and hypertension could influence its effectiveness. This reveals a gap in applicability, leaving clinicians with uncertainty in patient selection for RIPC. This study aims to lay the groundwork for tailored approaches in cardiac care by investigating these factors.
Methods
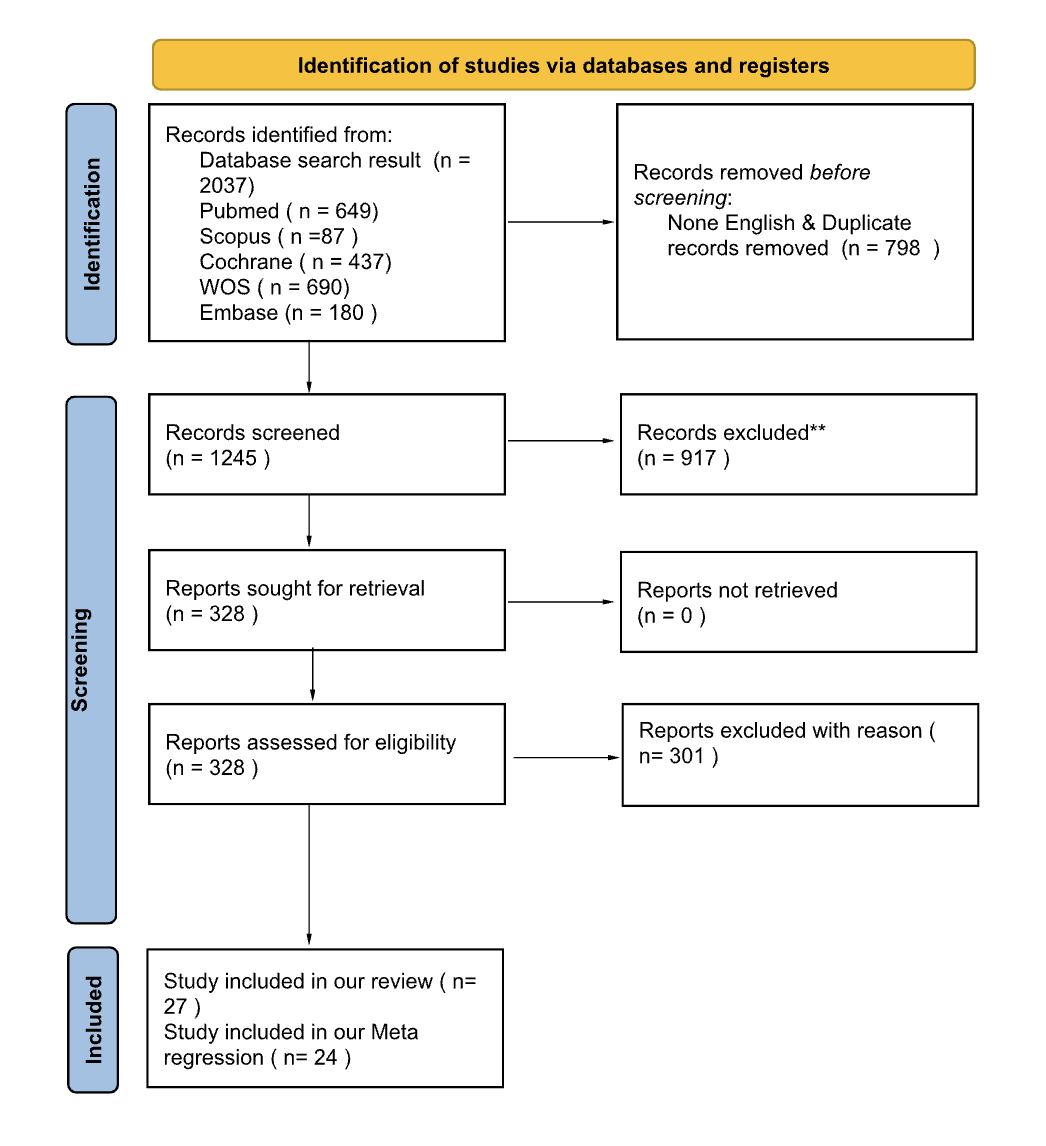
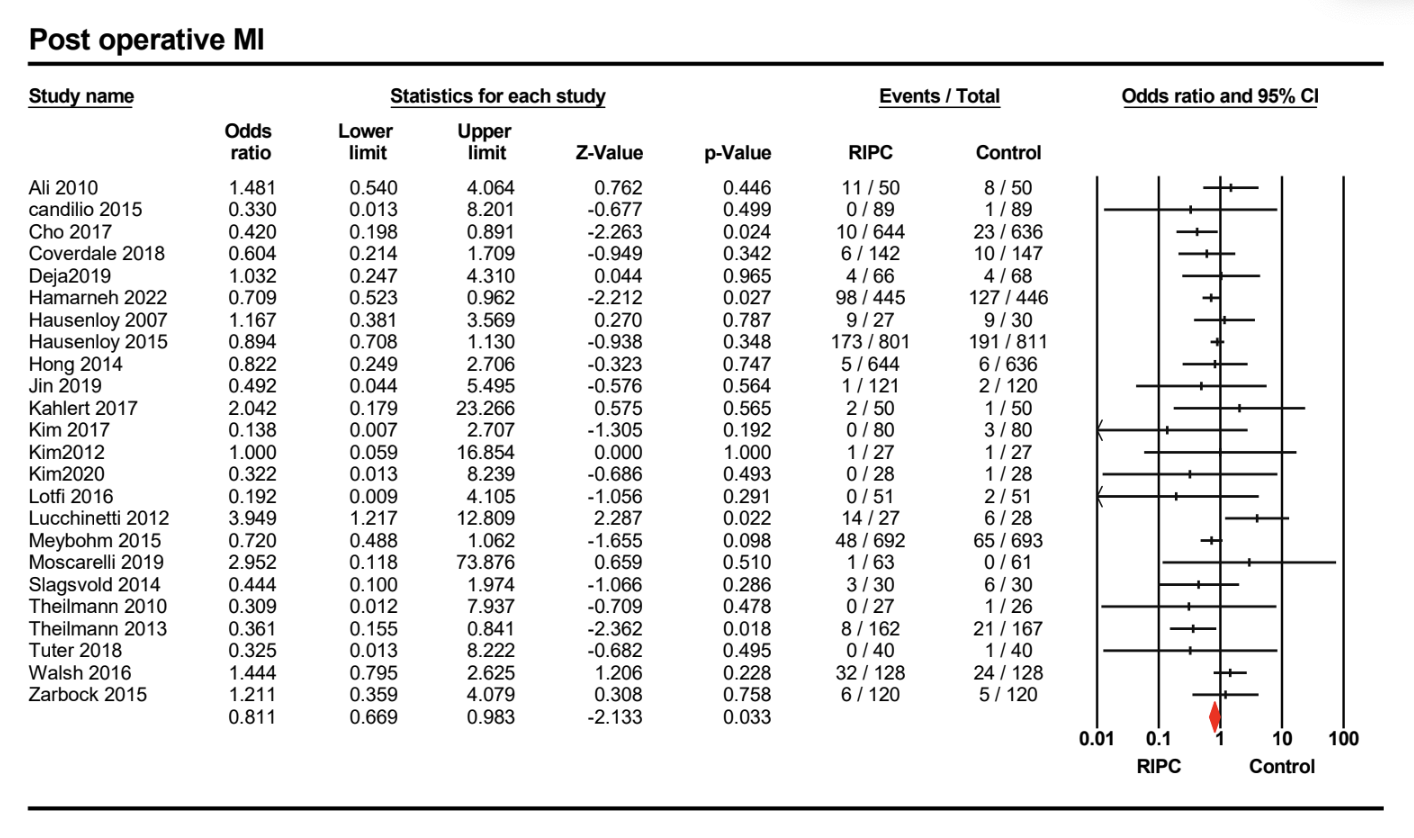
Methods: The Cochrane Central Register of Controlled Trials (CENTRAL), PubMed, MEDLINE (including MEDLINE InProcess) (OvidSP), Web of Science, Embase (OvidSP), and Scopus databases were searched from database inception until August 15th, 2023. We included randomized controlled trials confined to the English language that studied the effects of RIPC after cardiac surgery. In accordance with our search strategy, 1065 abstracts were reviewed, and 328 articles were selected for full-text screening after duplicates and irrelevant topics were removed as per PRISMA standards. A total of 24 studies were included for data extraction. Computations were performed using the Comprehensive Meta-Analysis Version 4 software. Using Cochrane tools for systematic reviews, the risk of bias, sensitivity analysis, and heterogeneity test were performed.
Results
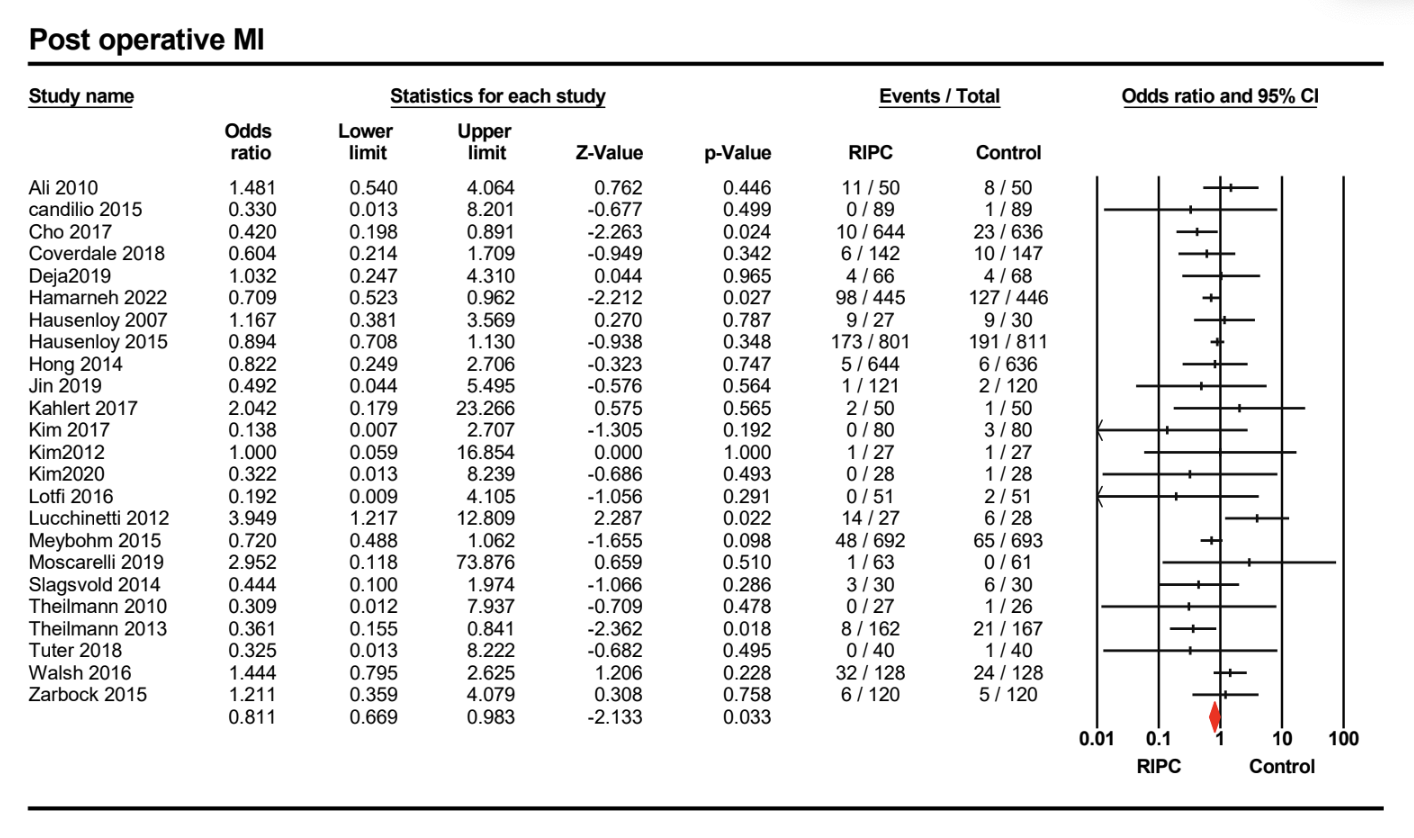
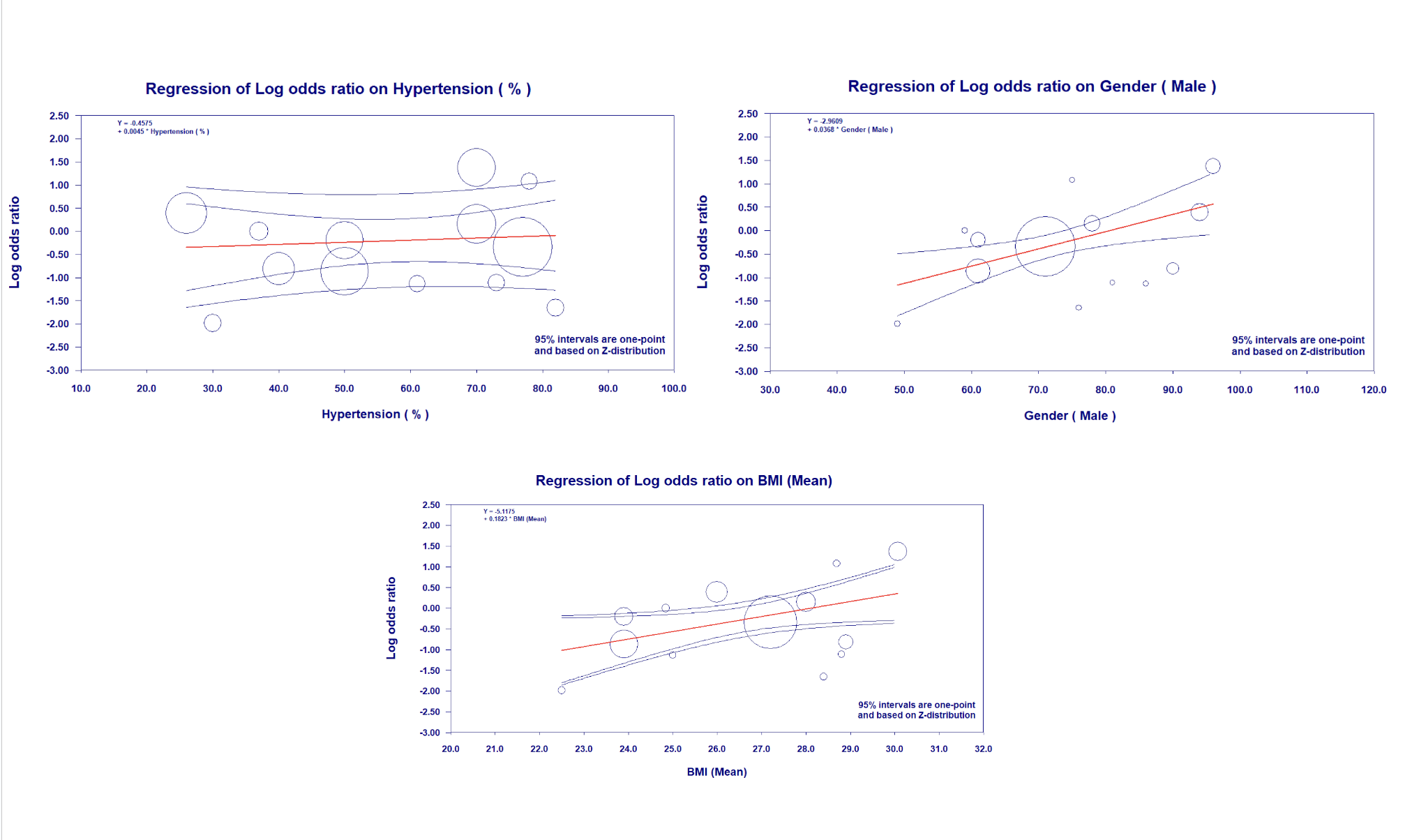
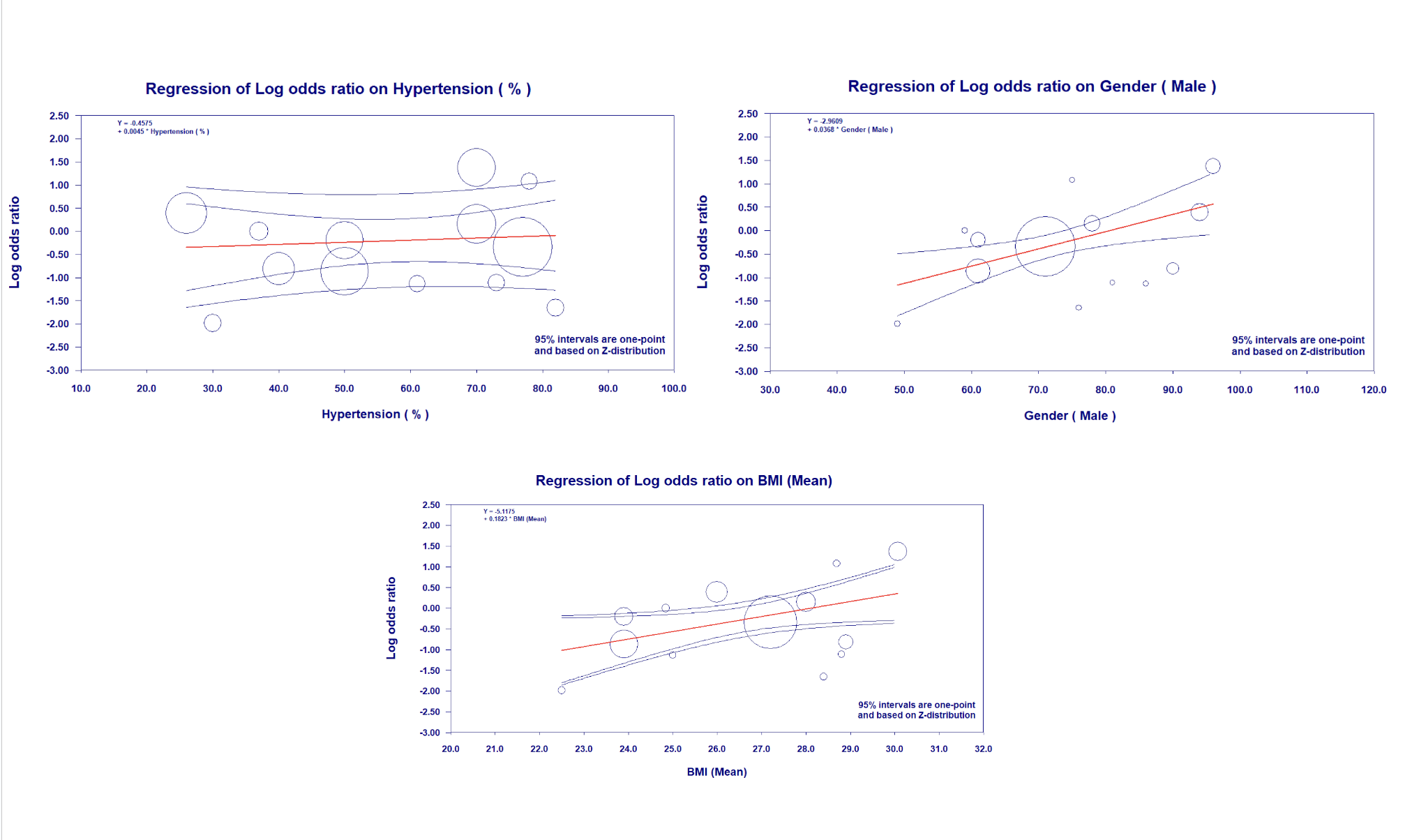
Results: A meta-analysis of 24 included studies demonstrated a significant reduction in the odds of postoperative myocardial ischemia with RIPC compared to the control (OR: 0.811; 95% CI: 0.669 to 0.983; p = 0.033). The reliability of this result across the included studies is reinforced by the low level of heterogeneity (I² = 0.143).Meta-regression findings: The meta-regression analysis showed that there is a significant association between mean BMI and the incidence of postoperative myocardial ischemia (Coefficient: 0.1823; 95% CI: 0.0104 to 0.3541; p = 0.0377). There was also a significant positive association between the percentage of males and the incidence of postoperative myocardial ischemia (Coefficient: 0.0368; 95% CI: 0.0108 to 0.0628; p = 0.0055). In contrast, hypertension does not have a significant effect on the incidence of postoperative myocardial ischemia following RIPC in cardiac surgeries (Coefficient: 0.0045; 95% CI: -0.0211 to 0.0301; p = 0.7307).
Conclusion
Conclusion: The study further strengthens the role of RIPC in reducing the risk of postoperative myocardial ischemia in cardiac surgeries. Our meta-regression analysis offers evidence that patient-specific factors significantly affect the risk of postoperative myocardial ischemia following RIPC. The data highlights a noteworthy association between mean BMI and gender with postoperative myocardial ischemia. The findings suggest that all-purpose RIPC protocols may be flawed, encouraging the development of tailored preconditioning regimens. This may improve the efficacy of RIPC, thus minimizing the incidence of myocardial ischemia and related complications. This study also recognizes gaps in our understanding of the mechanisms of these relationships, further inspiring future targeted research. The application of these findings into clinical practice could be an important step toward improving outcomes in cardiac surgery patients.