Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
CASE20200924_014
| Complex PCI - Chronic Total Occlusion | |
| Successful Rendezvous Technique with the Retrograde Approach for Chronic Total Occlusion After Anterograde Coronary Dissection | |
| Tung-Lin Tsui1, Shih-Chi Liu2 | |
| Camillian Saint Mary's Hospital Luodong, Taiwan1, Fu Jen Catholic University Hospital, Taiwan2, | |
|
[Clinical Information]
- Patient initials or identifier number:
303369
-Relevant clinical history and physical exam:
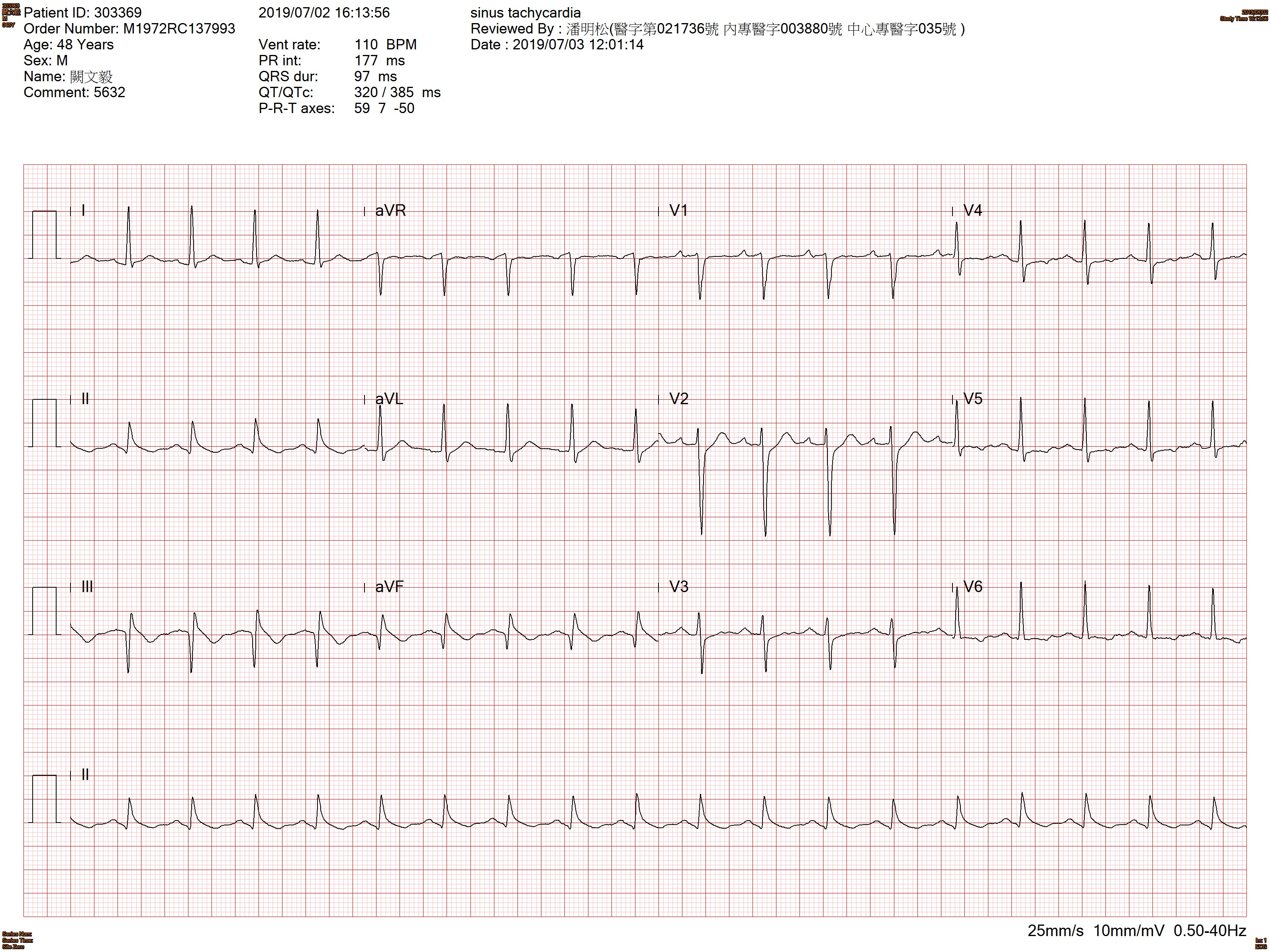
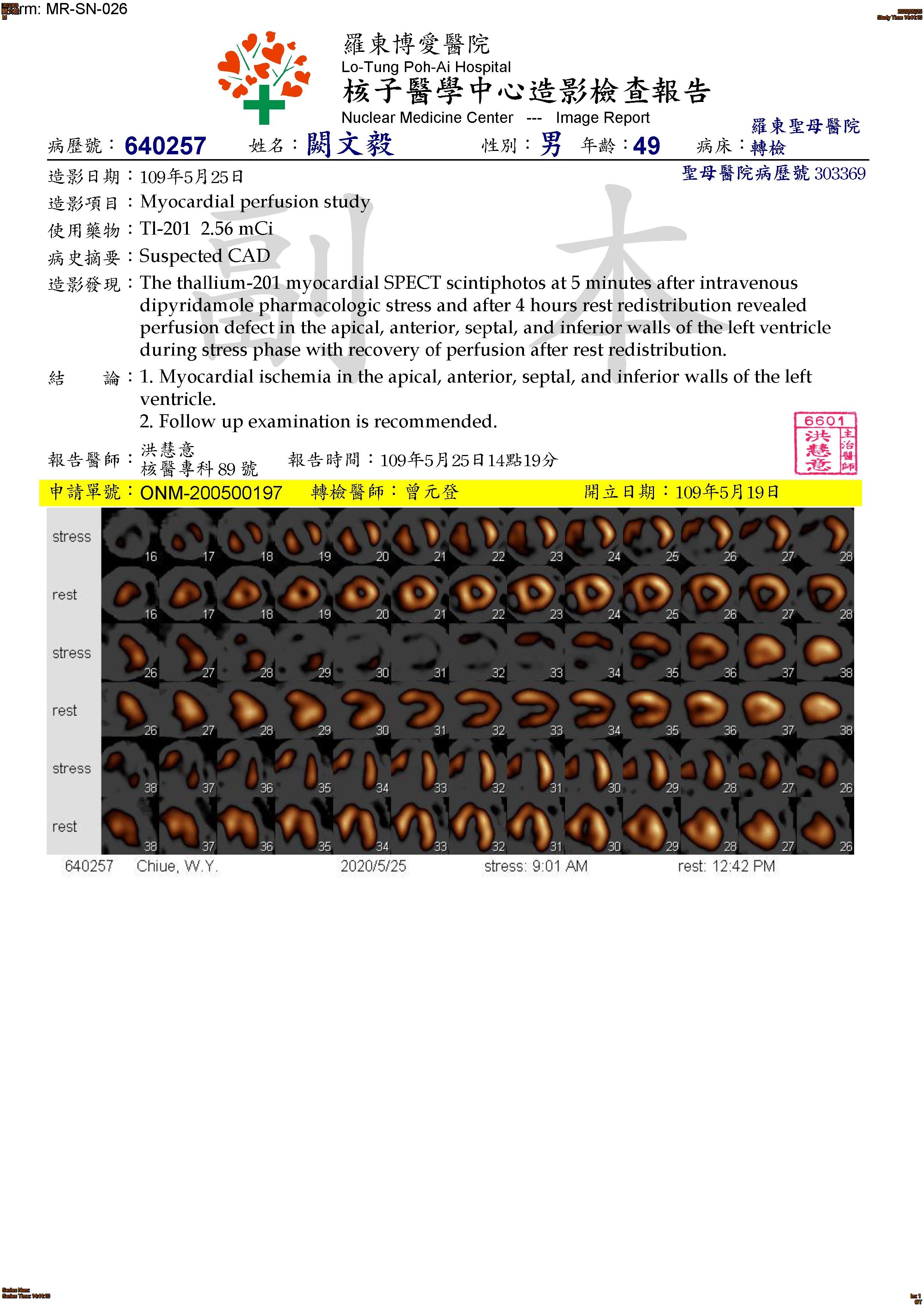
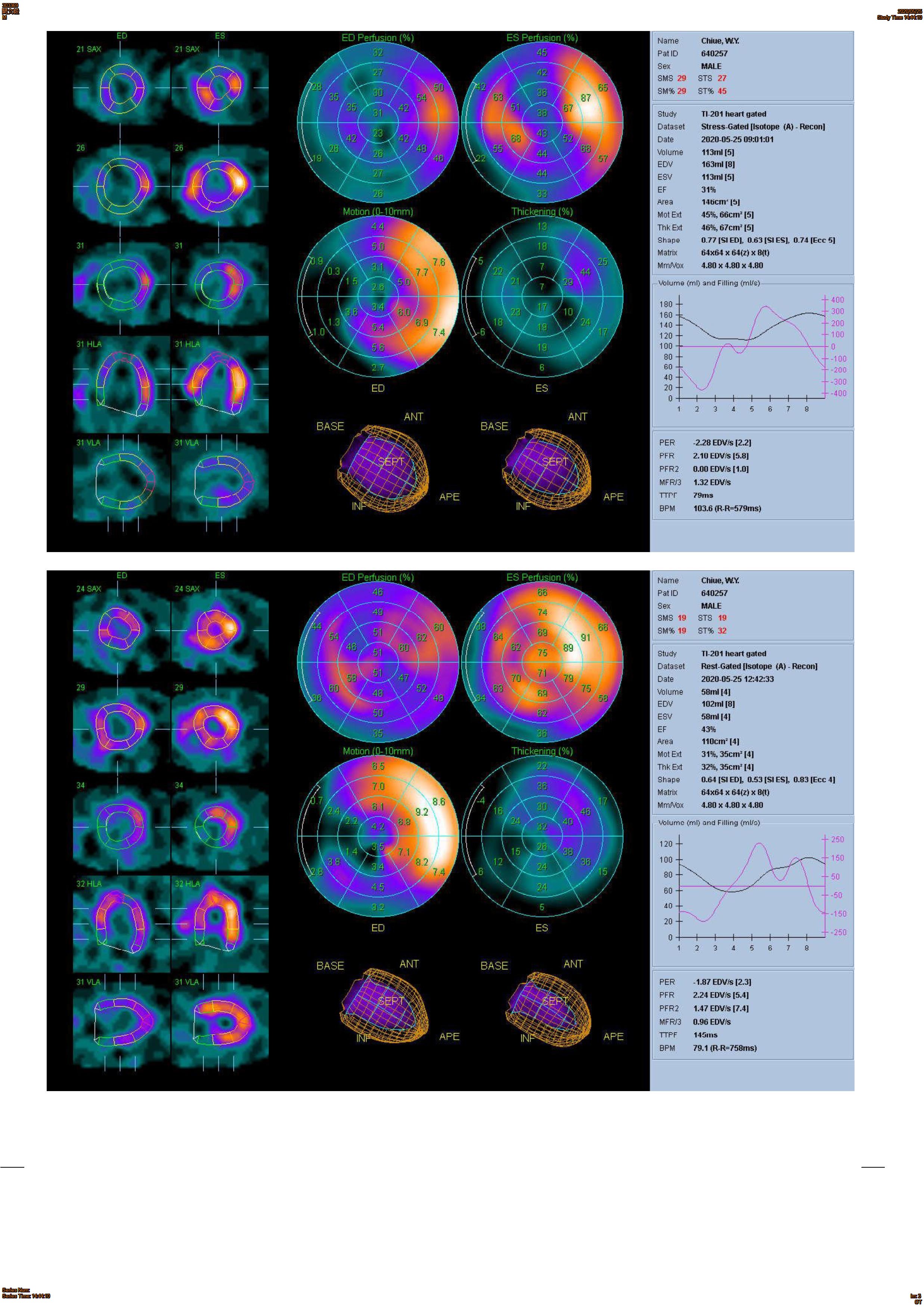
This 49 years old male, has history of hypertension, dyslipidemia and Ankylosing spondylitis under regular control at our CV + AIR OPD. He suffered from chest tightness for 6 months, associated symptoms with dyspnea, chest pain, cold sweating, palpitation and dizziness. He came to our CV OPD for help, thallium scan showed myocardial ischemia in the apical, anterior, septal, and inferior walls of the left ventricle. Under impression of suspected CAD. He was admitted to CV ward for further evaluation and management.
   -Relevant test results prior to catheterization:
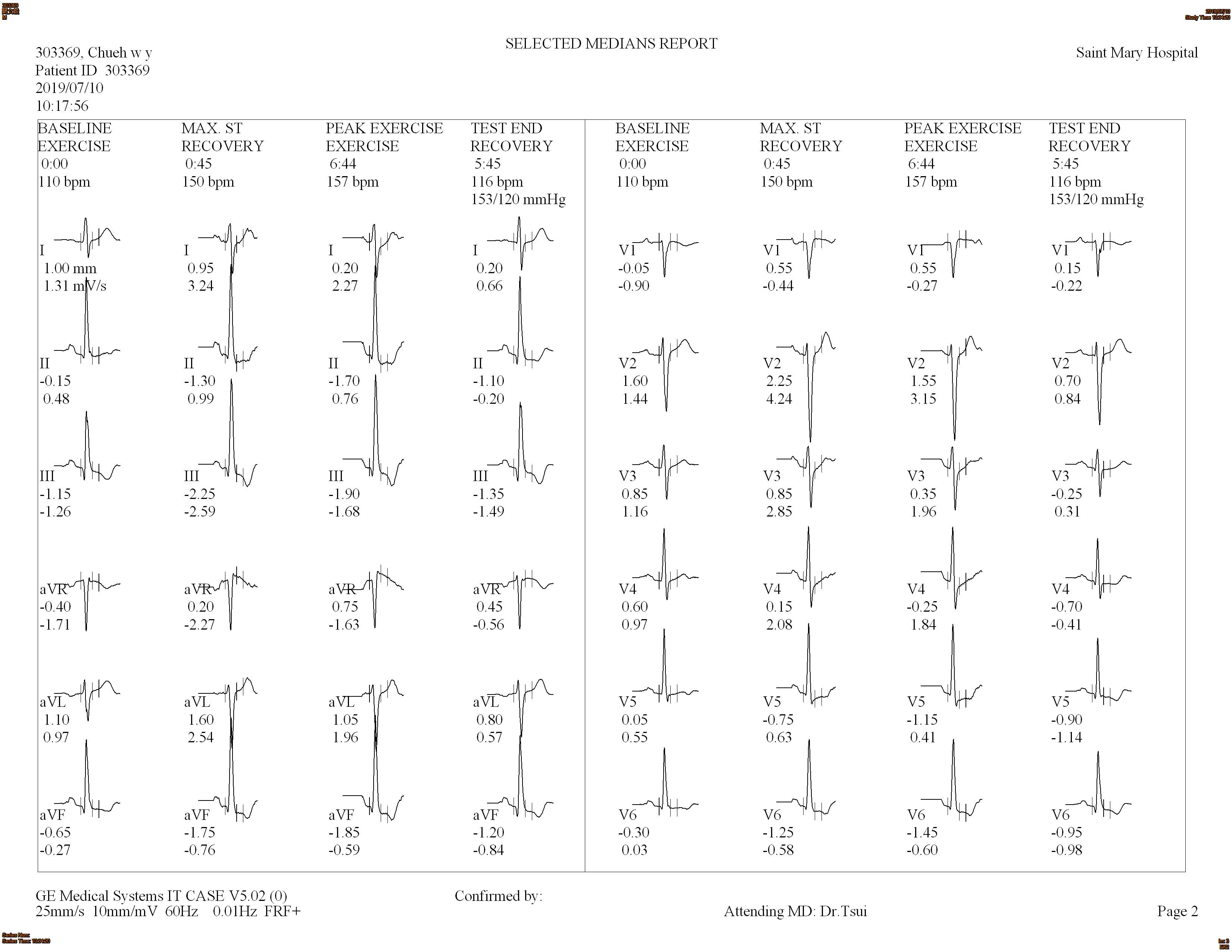
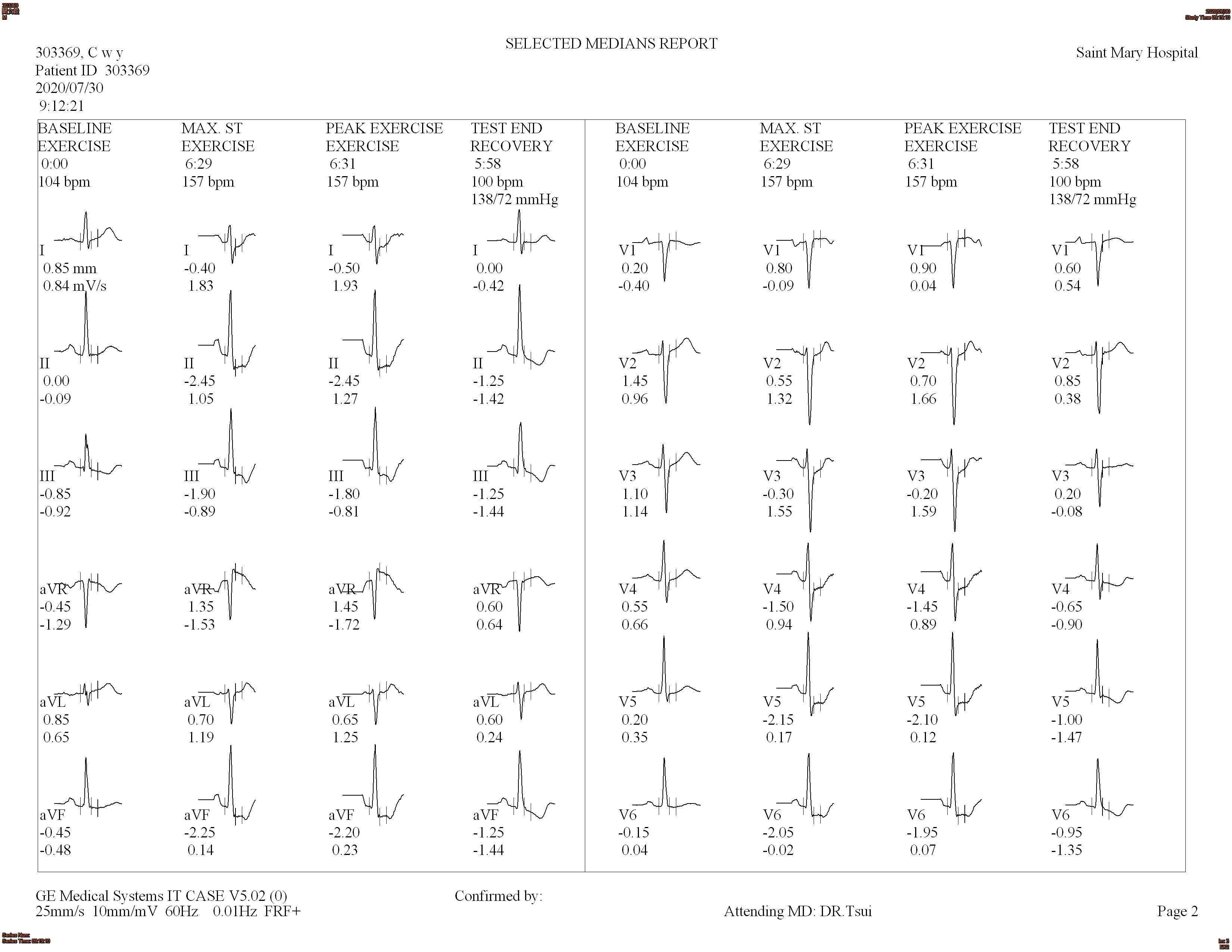
BMI around 25kg/m2. Hypertension with average blood pressure 160/96mmHg, dyslipidemia with LDL: 168, HDL: 29, Hba1c: 5.8, uric acid 9.7mg/dl. No legs edema, clear breathing sounds. Soft and flat abdomen. Extremities were all freely movable. The Treadmill exercise test showed positive with marked ST depression over inferior leads. The echocardiography study showed inferior wall hypokinesia. EKG showed Q wave over II, III, aVF. CXR showed mild cardiomegaly without lung congestion.
  - Relevant catheterization findings:
LAD: middle 95% stenosis with TIMI2 flow, D1 60% stenosis, septal 75% stenosis; LCX: proximal 50-60% stenosis with torturous vessel, OM 75% stenosis; RCA: middle 85% stenosis and distal 100% occlusion consider CTO, with small colateral circulation from left coronary artery. During PTCA for LAD, no antegrade flow after Floppy wire pass middle LAD lesion and severe angina was told. Rapidly balloon dilatation (3.0x10, 10 bars) and stent deployment (DES 3.0x38, 14 bars) was done. TIMI 3 flow with better colateral flow to PDA was noted.
|
|
|
[Interventional Management]
- Procedural step:
1. Via rightradial approach with AL1 GC, Antegradeapproach with Fincross microcatheter plus XTR and Gaia 1 wire, but failed tocross the lesion2. We changed wire to Conquest pro 12, and false lumen wascreated3. Left radial approach with EBU GC for LCA, Progreat microcatheter plus Gaia 2 wirefor septal branch wiring cannot arrived PDA via the septal branchfrom middle LAD. So we chose the septal branch from distal LAD with Progreat plus Fielder FCwire4. Progreat delivered to distalseptal branch near PDA, and changed wire to Gaia 2, and wired to PDA anddistal RCA5. Progreat delivered todistal RCA, changed wire to Conquest pro 12, and wired to middle RCA,and Progreat was delivered to middle RCA6. We changed the wire to Floppywire and it was wired to proximal RCA, andrendezvous technique by tip-in method, with extension wire, the retrograde Floppy wire was wired into the antegrade fincross very well7. The antegrade fincross was delivered toPDA and the retrograde Progreat was moved back to PDA, we wired theFielder FC wire via antegrade approach, and retrieved the retrograde wiregently8. After balloon dilatation with 1.0x5 and 2.5x15,IVUS was delivered to PDA and move back to proximalRCA, 2.8mm diameter for distal lumen with long dissection was found9.A BIOMIME MORPH 3.0-2.5-60mm DES was deployedover proximal to distal RCA supported by guidelinear10. After DES 3.0x32 and 2.5x32 for OS to P RCA and PDA and NC 3.0x20 for post dilatation, we got TIMI 3 RCA flow.
- Case Summary:
The antegrade flow from proximal to distal RCA is notonly a critical stenosis but a CTO lesion with brushing colateralcirculation. Retrograde approach may be more helpful to find true lumen. For complex PCI for CTO lesion, we needed special wires and microcatheters to pass different lesions which have their own characteristics. There is no unique perfect wire can pass all CTO lesion. If antegrade microcatheter can be delivered into the colateral channel, we can do the Re-wipe method, however, if we can wire the retrograde wire into the antegrade microcatheter in GC, Tip-in method will be useful. In some cases, deliver OTW balloon via retrograde wire and do CART method may be efficient.
|
|