Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
CASE20200924_009
| Adjunctive Procedures (thrombectomy, artherectomy, special balloons) - Adjunctive Procedures | |
| Managing Complication of Orbital Atherectomy in Calcified Lesion | |
| Shargunandass Iynam1 | |
| Hospital Serdang, Malaysia1, | |
|
[Clinical Information]
- Patient initials or identifier number:
WYC
-Relevant clinical history and physical exam:
68 year old lady with 1. Dyslipidemia (on T. Atorvastatin)2. Right Breast Cancer (Mastectomy done 10 years ago and no recurrence) 3. Ischemic Heart Disease in March 2020 (NSTEMI)- Coronary Angiogram revealed three vessel disease.- Urgent PCI to RCA (uncomplicated) done, planned for staged PCI to LAD with Orbital Artherectomy.
Remains asymptomatic since first PCI. Compliant to DAPT.Echocardiogram shows preserved EF, good LV function, no motion abnormalities Clinical examination : normal -Relevant test results prior to catheterization:
ECG : Sinus rhythm, Rate 88, Normal axis, No ischemic changes, normal intervals and segments
Chest X-ray : no Cardiomegaly, clear lung fields Hb: 12.6 g/dL Plt : 193 T. Cholesterol : 4.08mmol/L TG : 0.90 mmol/L LDL : 2.09 mmol/L HDL 1.58mmol/L HbA1C : 5.3% Creatinine : 67umol/L Urea : 6.8 Sodium: 137 Potassium: 4.1 PT: 14.2 sec aPTT 30.1 sec INR 1.08 - Relevant catheterization findings:
Coronary Angiogram March 2020Approach: RadialLMS : Ostial LMS 20% stenosisLAD : proximal 80% with calcificationsLCx: Proximal 80% stenosis at bifurcation of OM1RCA : Ostial RCA 95% stenosis at, Proximal 80% stenosis, 90% at bifurcation PDA/PLVImpression : Tripple vessel disease
PCI to RCA was done during this setting as shown in attachmentPLV and PDA was treated with drug-coated balloon 2.25 mm X 30 mmOstial to proximal RCA treated with drug-eluting stent 3.0 mm X 48 mm |
|
|
[Interventional Management]
- Procedural step:
Staged PCI to LAD with Orbital Artherectomy (Diamondback, CSI) and Optical Coherence Tomography (OCT) guidance was done in August 2020.
Left Main Stem was engaged with EBU 3.0 guiding catheter.Rinato coronary wire was crossed into LAD.OCT catheter (Dragonfly, Abbot) was unable to be passed through the tight and calcified LAD.Decided to proceed with Orbital Artherectomy without diagnostic intracoronary imaging. Orbital Artherectomy was done carefully with some resistance felt initially while passing through the burr (Total 3 runs, the first two at 80,000 rpm and last run at120, 000 rpm).Patient stable throughout procedure. Post Artherectomy, noted severe mid LAD DISSECTION AND LARGE HEMATOMA. Decision made to immediately deploy stent at the region to avoid further propogation of dissection and hematoma, which can leave disastrous and potentially fatal consequences. Mid-LAD stented with DES 3.0 mm X 30 mm and ostium to mid-LAD with DES 3.5 mm X 26 mm Post PCI angiogram shows no more dissection or hematoma and TIMI 3 flow was established. Post-dilated LAD with Non-Compliant balloon 3.0 mm X 30 mm and 3.5 mm X 15 mm at maximum 16 atm. Post PCI OCT shows good stent apposition and no residual dissection or hematoma or edge dissections with proximal stent MSA 10.73 mm2 and distal stent MSA 5.09 mm2. Patient was stable throughout procedure. 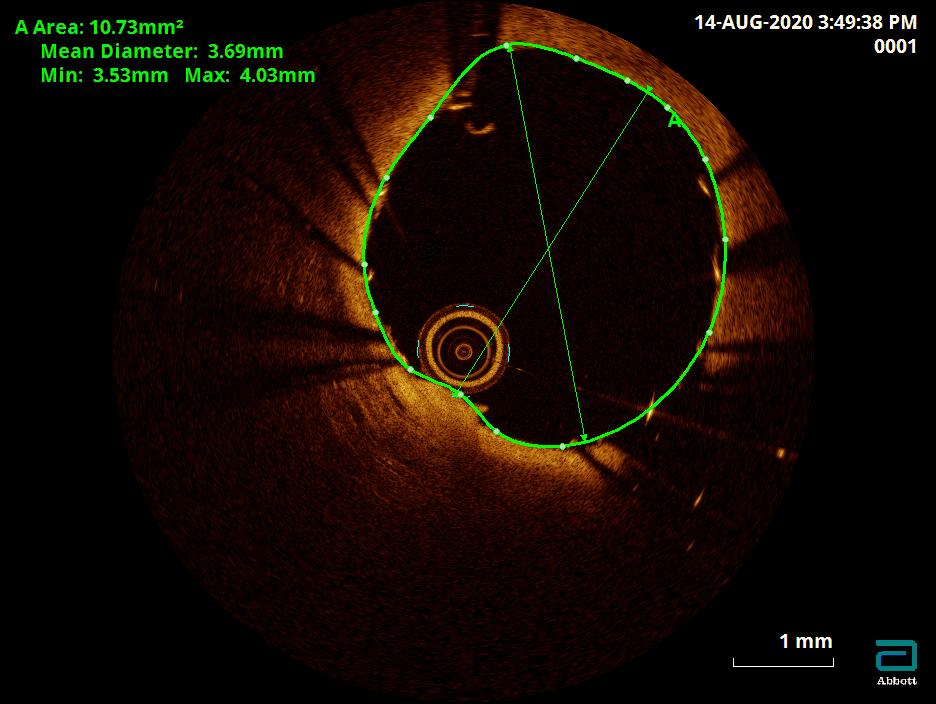 - Case Summary:
1. Artherectomy is an effective lesion preparation strategy for calcified lesions.2. An important advantage of orbital artherectomy is more calcium modification in lesions with larger lumen area, more noncalcified plaque modifications & lesser fluoroscopy time (Yamamoto MH et al and S. Geol et al).3. Orbital artherectomy produces higher rates of device-induced perforation as reported by S. Goel et al in a meta-analysis.4. Large dissections and hematomas need to be managed promptly with intervention and supportive therapy to avoid further progression including perforation.5. OCT-guided interventions produce excellent immediate and long term outcomes in complex cases and complications.
|
|