Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
CASE20200912_092
| Complications - Complications | |
| Life Threatening Coronary Artery Dissection Post Drug Coating Balloon in a Very Young Patient with NSTEMI | |
| Heng Shee Kim1, Mahadevan Gurudevan2, Benjamin Leo Cheang Leng3, Chuey Yan Lee4 | |
| Sultanah Aminah Hospital, Malaysia1, Sultanah Amina Hospital, Malaysia2, Columbia Asia Hospital Tebrau, Malaysia3, Hospital Sultanah Aminah, Malaysia4, | |
|
[Clinical Information]
- Patient initials or identifier number:
Vad
-Relevant clinical history and physical exam:
A 24-year-old man with no past medical history presented with typical angina chest pain. He has no cardiovascular risk factor except a chronic smoker of 10-packs-year. Physical examination was unremarkable.
-Relevant test results prior to catheterization:
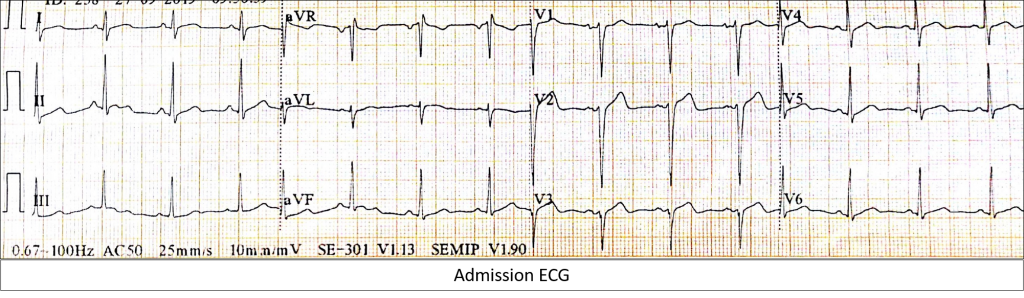
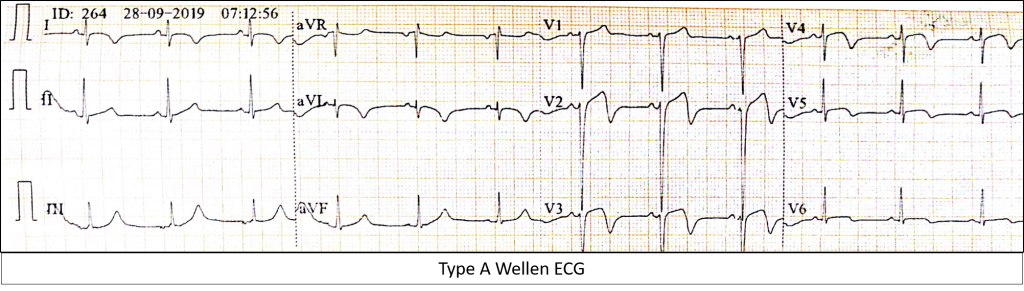
ECG showed progressive T-inversion indicating Wellen's Type A ECG over the anterolateral lead with elevated hsTrop-T. He was treated as NSTEMI with DAPT and fondaparinux. He was planned for in-patient CAG.
  - Relevant catheterization findings:
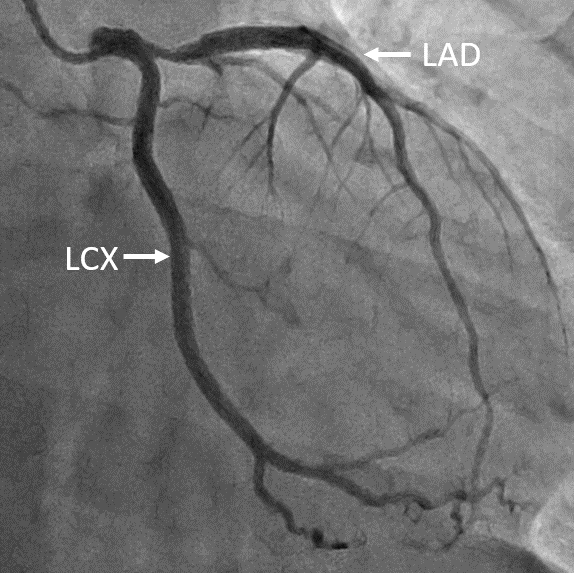
CAG showed 80%stenosis of ostial LAD with normal LCx and RCA. In view of young age, we decided for DCB strategy if feasible afterlesion preparation, keep in view bailout with DES or emergency CABG.
 |
|
|
[Interventional Management]
- Procedural step:
He was brought in for emergency CAG with XB 3.5 7F, noticed ATO of ostial LAD. LAD was wired with BMW II, LCX PT II. Few rounds of thrombus aspiration were performed but failed to aspirate any thrombus and remained in TIMI 0 flow. Ostial LAD pre-dilated with 3.0x15 SC, noted only TIMI I flow. We decided to stent LM to pLAD with 4.0x38 DES. While post-dilating left main, he developed VF. The stent balloon immediately deflated and CPR performed. He regained full GCS after 2cycles of defibrillation and CPR. Repeat CAG showed TIMI III flow. LM-LAD stent further post-dilated with NC 4.5x10 up to 18atm. He was well post-procedure with unsupported vital signs and resolution of ST-elevation. His echocardiogram showed good function with no wall abnormalities. 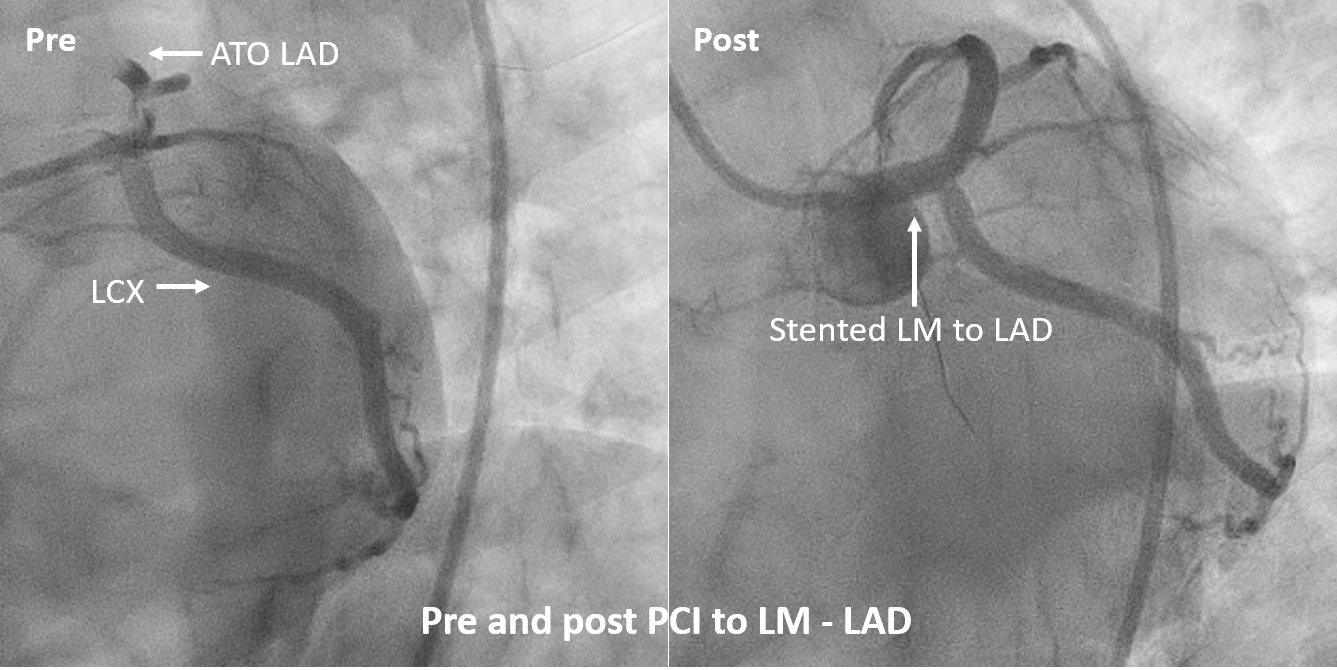 - Case Summary:
Management of CAD in very young patients remains challenging, and this case illustrates the dilemma in treating this group of patients with DCB vs DES strategy. Besides, our case also demonstrated the almost life-threatening progression of benign coronary artery dissection (Type A-B) to acute total occlusion of the coronary artery. Vigilant post-PCI monitoring of this group of patients remains relevant. |
|