Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
CASE20200831_001
| Imaging - Invasive Imaging (IVUS, OCT, spectroscopy, etc) | |
| Tip Detection Method Adapted for Non-CTO Complex Lesions During Intravascular Ultrasound-guided Coronary Intervention | |
| Satoshi Suzuki1, Atsunori Okamura2, Hirokazu Tanaka1, Kota Tanaka1, Akinori Sumiyoshi3, Hiroyuki Nagai4, Mutsumi Iwamoto1, Satoshi Watanabe1, Kenshi Fujii1 | |
| Sakurabashi Watanabe Hospital, Japan1, Sakurabashi Watanabe Advanced Healthcare Hospital, Japan2, Sakurabashi Watanabe Advanced Health care Hospital, Japan3, Saint Joseph's Translational Research Institute, USA4, | |
|
[Clinical Information]
- Patient initials or identifier number:
EK,TK,MM
-Relevant clinical history and physical exam:
We want to present 3 cases which were difficult in non chronic total occlusion percutaneous coronary intervention due to chest pain. First case was 89 years old male and second case was 78 years old male and third case was 69 years old male. They had effort angina without electrocardiogram change.
-Relevant test results prior to catheterization:
- Relevant catheterization findings:
|
|
|
[Interventional Management]
- Procedural step:
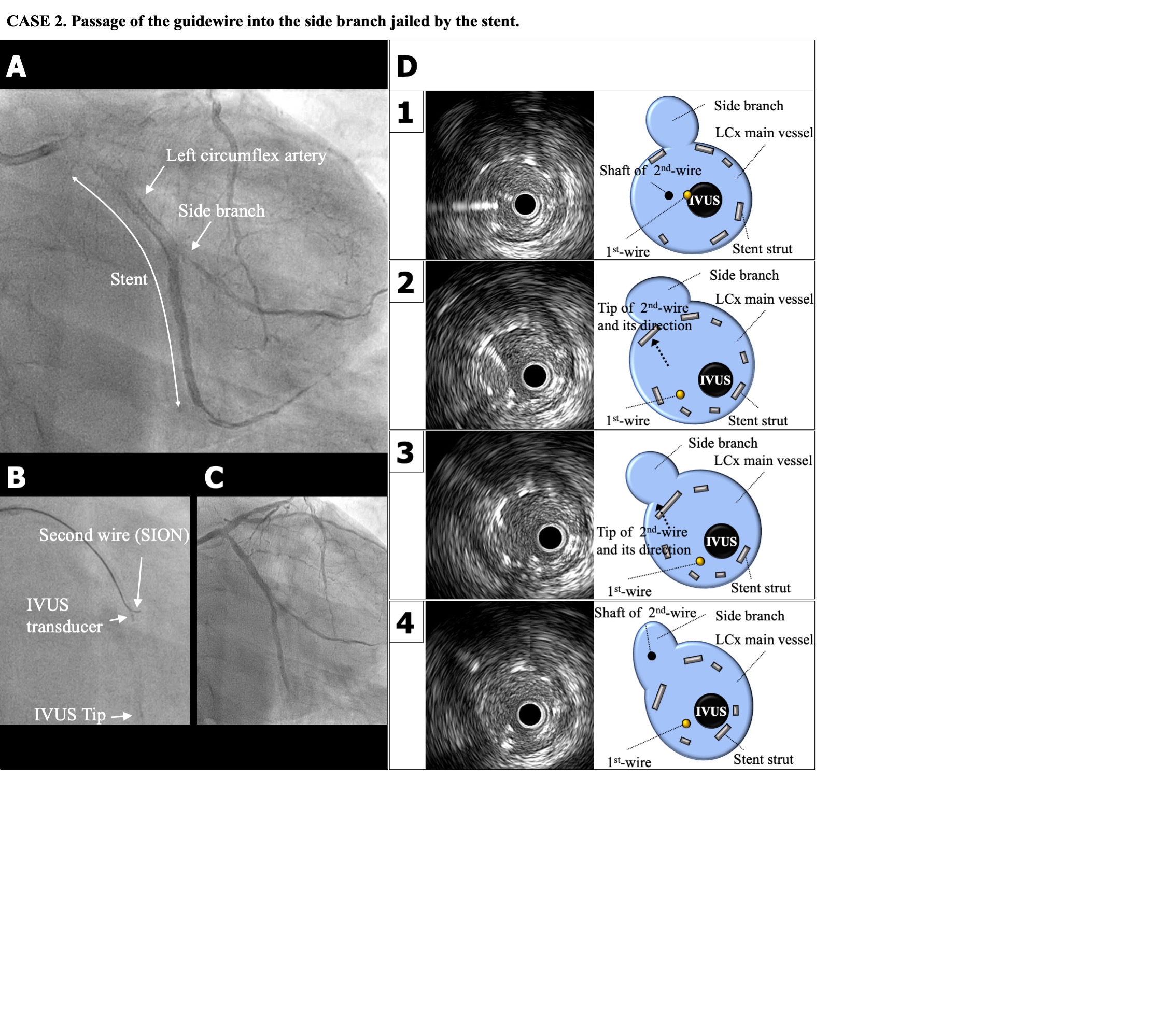
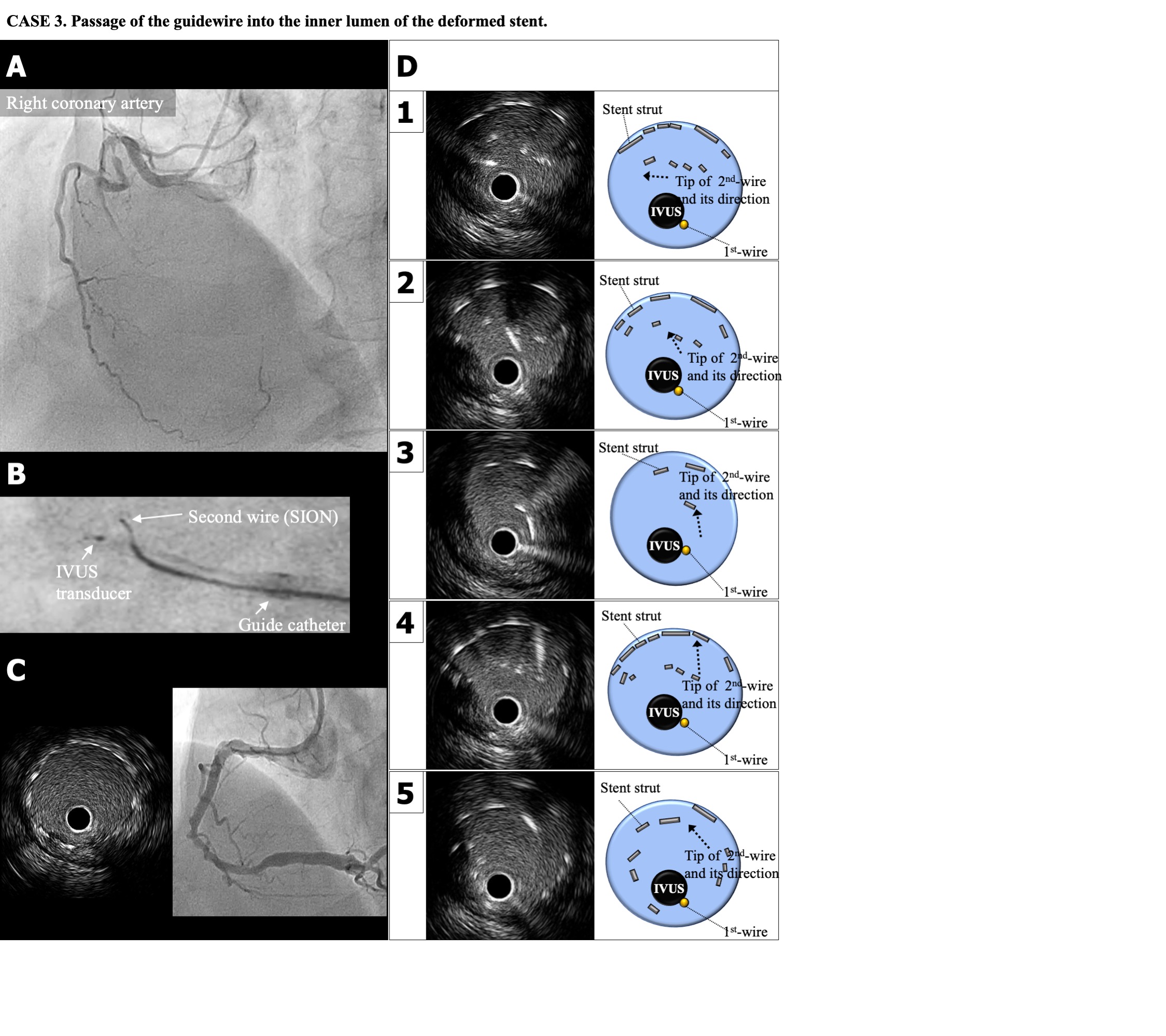
CASE1:IVUS observations from the diagonal branch showed that the entrance of the stenotic lesion in the LAD was at 11 – 12 o¡¯clock (CASE 1D-1). Using the tip detection method, the tip of the guidewire was accurately directed to the entrance of the stenotic lesion (1D-2), and advanced while being rotated clockwise from 9 o¡¯clock (1D-3) to 1 o¡¯clock (1D-4). The guidewire was successfully passed through the lesion, followed by stenting (1C).CAE2:Under angiographic guidance, a SION guidewire could not be entered into the side branch because it was jailed by the stent. AltaView IVUS observation from the main branch showed that the entrance to the side branch was located at 11 – 12 o¡¯clock (CASE 2B, 2D-1). Using the tip detection method, the tip of the guidewire was accurately directed to the entrance of the side branch (2D-2). The tip was advanced in the correct direction (2D-3) and the shaft of the guidewire was navigated into the branch (2D-4).CASE3 was navigation of the guidewire into the inner lumen of the deformed stent. There was a subtotal lesion at the proximal part of the right coronary artery (RCA) (CASE 3A). After stent implantation of a 3.5 ¡¿ 28-mm stent, a 4 ¡¿ 15-mm balloon for postdilation could not be entered into the stent because the proximal site of the stent was malapposed against the vessel wall and both the SION guidewire and guide catheter were pushed out of the RCA. Finally, In-stent route was gained by tip detection method.
   - Case Summary:
The three cases presented here demonstrated that the tip detection method was useful in non-CTO PCI procedures requiring accurate guidewire control. The tip detection method is very useful not only for CTO lesions, but also for complex non-CTO lesions through which it is difficult to pass the guidewire.
|
|