Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
CASE20191118_001
| CORONARY - Complex and Higher Risk Procedures for Indicated Patients (CHIP) | |
| Cardiogenic Shock in a Patient with Severe AS and TVD | |
| Jonathan Xinguo Fang, Frankie CC Tam3, Cheung Chi Simon Lam3, Anthony Yiu Tung Wong4 | |
| , Queen Mary Hospital, Hong Kong, China3, Hong Kong Sanatorium & Hospital, Hong Kong, China4, | |
|
[Clinical Information]
- Patient initials or identifier number:
CKY
-Relevant clinical history and physical exam:
88-year-old lady with history of diabetes, hyperlipidemia, hypertension, and history of moderate aortic stenosis on echocardiogram 5 years ago presented with acute onset dyspnoea and chest pain for 1 day. On examination, she was in respiratory distress. Bilateral crepitations and wheeze were audible in both lung fields. The jugular venous pressure was elevated. There was 1+ ankle edema. There was pulsus parvus et tardus, tachycardia, and an ejection systolic murmur at the aortic area
-Relevant test results prior to catheterization:
ECG showed sinus tachycardia with ST elevation in aVR and ST depression in aVL, I, V2-V6. Left-main-equivalent disease was suspected. CXR showed acute pulmonary edema. high sensitivity Troponin T (Roche) was around 2000. Echocardiogram showed severe AS. Concentric LVH and preserved LVEF~55%. The diagnosis of NSTEMI with acute pulmonary edema/Killip III, Left-main-equivalent disease and severe aortic stenosis was made. 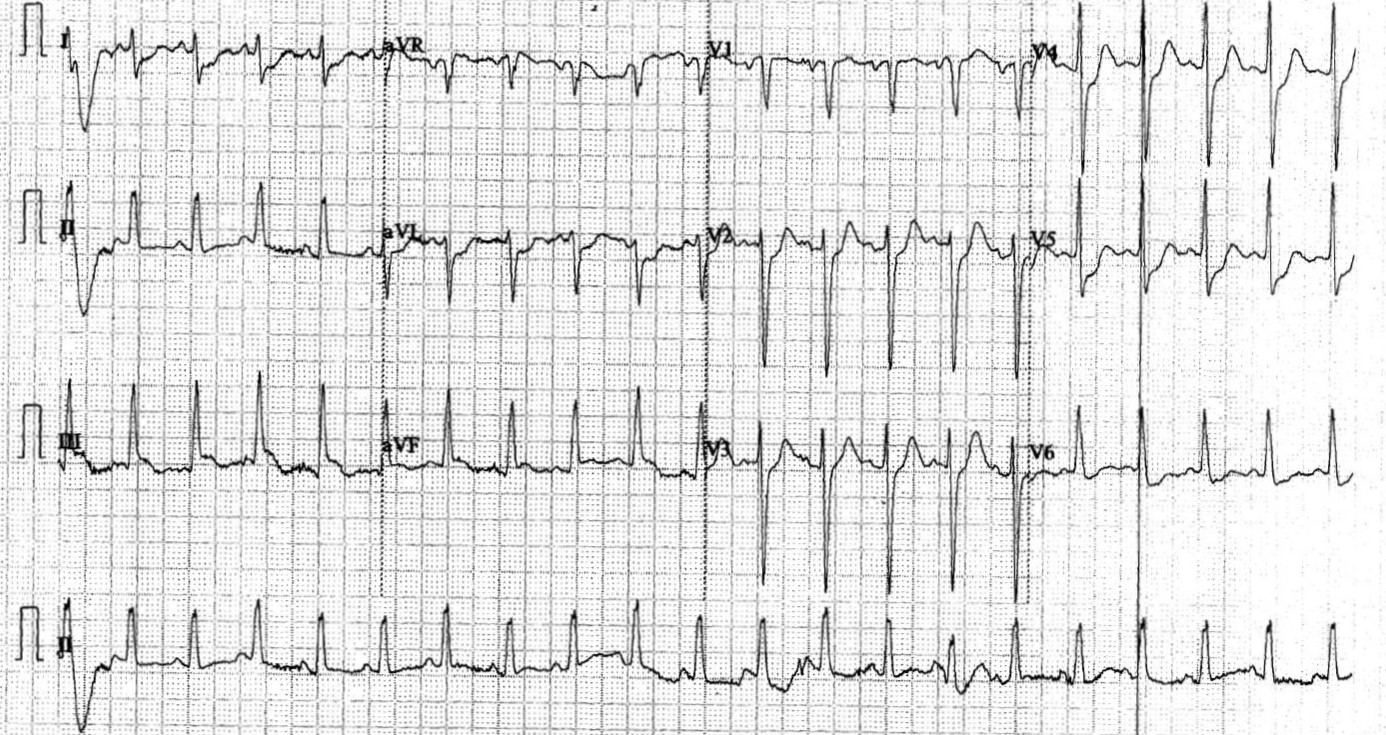 - Relevant catheterization findings:
Severe AS coronary: left dominance. Left main minor disease LAD pLAD critical 90% disease. calcified disease LCx mLCX critical 90% disease RCA mRCA CTO with right-to-right collaterals Aortogram and bilateral femoral arteriogram were done. The patient was deemed inoperable after heart team decision. Decided for PCI and transfemoral TAVR |
|
|
[Interventional Management]
- Procedural step:
PCI to LCx LFA 7Fr EBU 3.5 guiding, Runthrough HC and SION blue GW to LCx and OM. 2.0 NC scoring balloon to LCx and 2.0 NC balloon to POBA OM. LCx stent with 2.5/39 DES. postdilate with 3.0 NC balloon at 18atm. KBI at LCx/OM with NC 3.0/2.0. IVUS. PCI to RCA CTO: 7Fr JR4. Corsair pro MC antegrade wire Fielder XTA entered subintimal space. Parallel wiring with Gaia 2nd on Caravel MC entered true lumen. Switched to Sion Blue. predilate with 2.0 balloon, Stent with 3.0/28 , 3.5/29, 4.0/32 DES. Postdilate with NC 3.5 at 20atm and NC 2.0 at 16atm. IVUS result good. BAV Planned for staged PCI to LAD and TAVI but patient developed cardiogenic shock. LFA 6Fr sheath Balloon valvotomy to AV with 14mm Nucleus then 16mm Nucleus balloon under rapid pacing. Postvalvuloplasty AV gradient 30/14mmHg. Mild AR. Staged PCI to LAD/shockwave. XB LAD 3.5, Terumo RT HC. IVUS guided. IVUS showed circumferential Calcium, mLAD and ruptured plaque in LM. mLAD predilate with 2.0/15, 3.5/10 scoring balloon. Shockwave lithotripsy balloon 2.5/12 at mLAD for 3 cycles. Shockwave balloon ruptured on 4th cycle. 46 pulses given in total at 4atm/6atm. Excellent balloon expansion. p-mLAD stent 3.0/33 DES, postdilate with 3.0/15 NC balloon. LM/LAD predilate with 4.0/15 balloon, stent with 4.0/28 DES, postdilate with NC 5.0/12 balloon. Excellent angiographic and IVUS result. TF TAVR LFA 6Fr LFV 6Fr RFA 10Fr. AV cross with Emerald, exchange to Safari. Rapid pacing. SAPIEN 3#23mm -2ml deployed. TEE showed trivial AR. - Case Summary:
This case demonstrates successful management of a patient with severe AS TVD NSTEMI with cardiogenic shock with PCI to triple vessel including shockwave lithotripsy to pLAD calcified lesion and emergency balloon aortic valvotomy followed by early staged transcatheter aortic valve implantation.
|
|