Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
CASE20191107_002
| CORONARY - Acute Coronary Syndromes (STEMI, NSTE-ACS) | |
| Nightmare in Primary PCI in a Patient with High Thrombus Burden: Combating with ¡®Slow Flow¡¯ After Thrombus Aspiration | |
| Siew Hoon Ong1, Nay Thu Win2, Azmee Mohd Ghazi1, Amin Ariff Nuruddin1 | |
| National Heart Institute, Malaysia1, Royal Free London, United Kingdom2, | |
|
[Clinical Information]
- Patient initials or identifier number:
WN, 413393
-Relevant clinical history and physical exam:
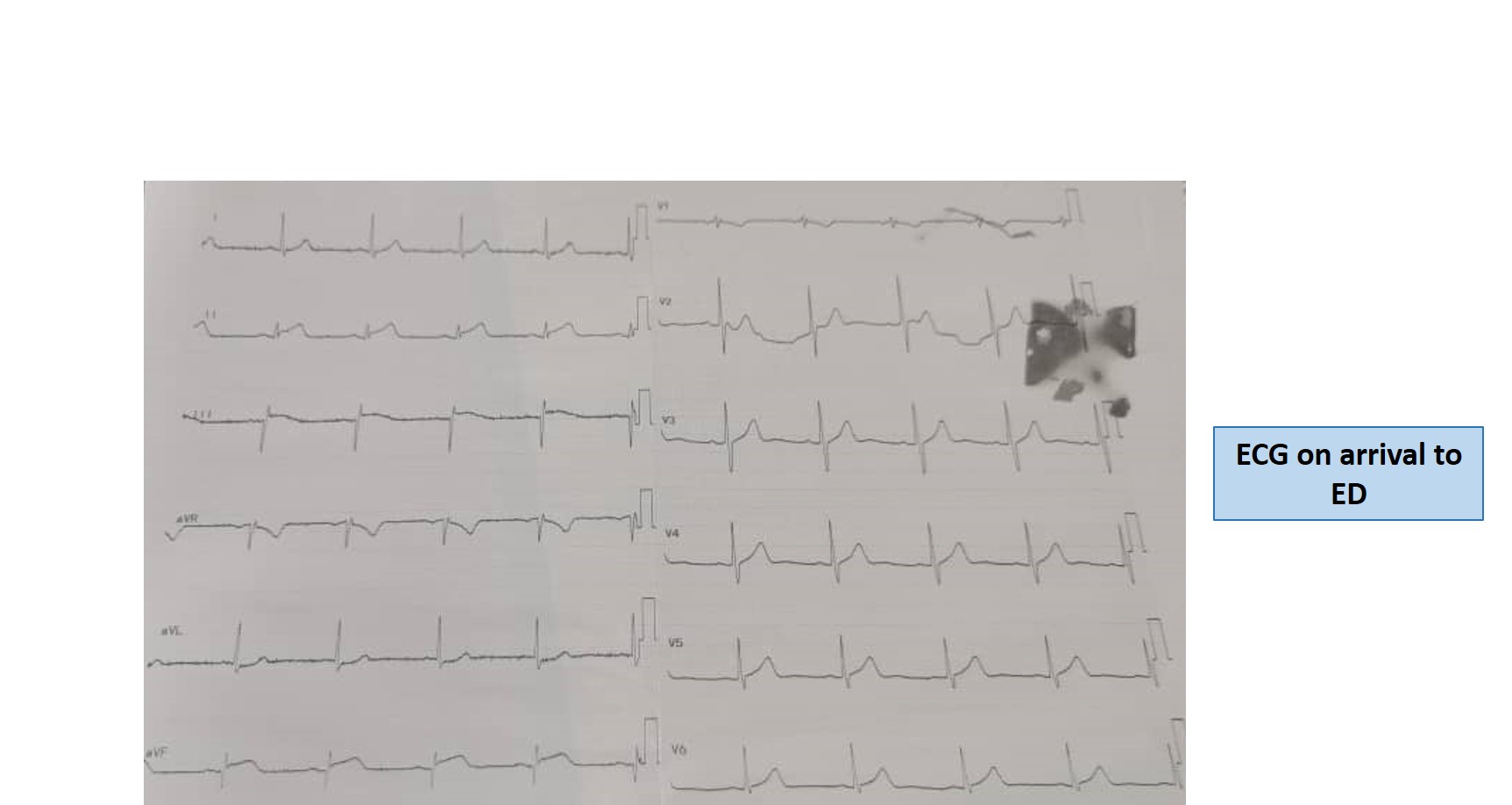
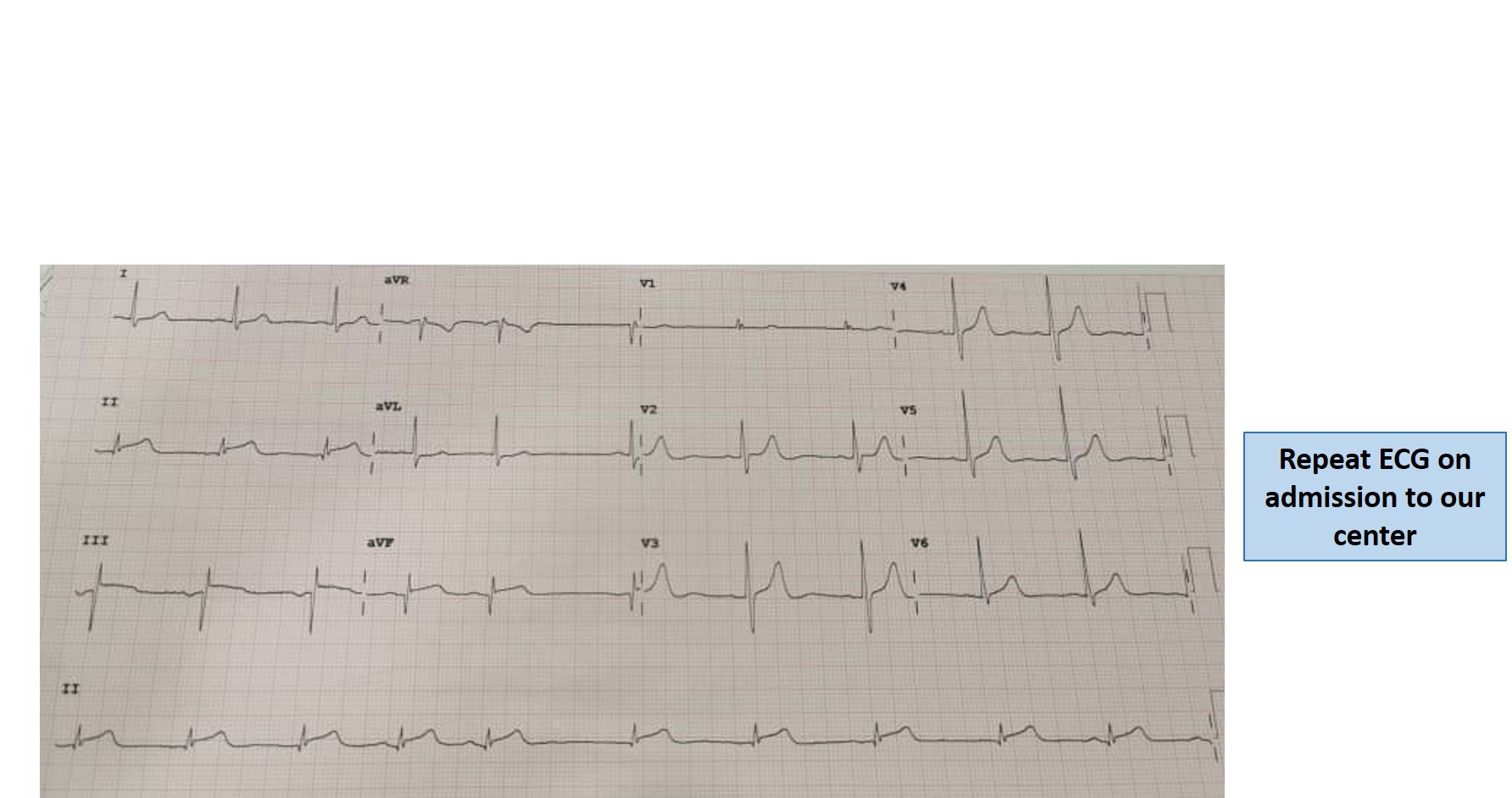
A 63-year-old gentleman with underlying hypertension, diabetes mellitus and dyslipidemia presented with central chest pain 4 hours prior to non-PCI capable center. The chest pain was associated with shortness of breath, diaphoresis and giddiness. ECG showed ST elevation at the inferior leads. He was referred immediately to our center for primary PCI.
-Relevant test results prior to catheterization:
Laboratory data showed creatinine 113umol/l, hemoglobin A1c 6.1%, NT-pro-BNP 113 pg/ml, Troponin-T 2161pg/ml.
  - Relevant catheterization findings:
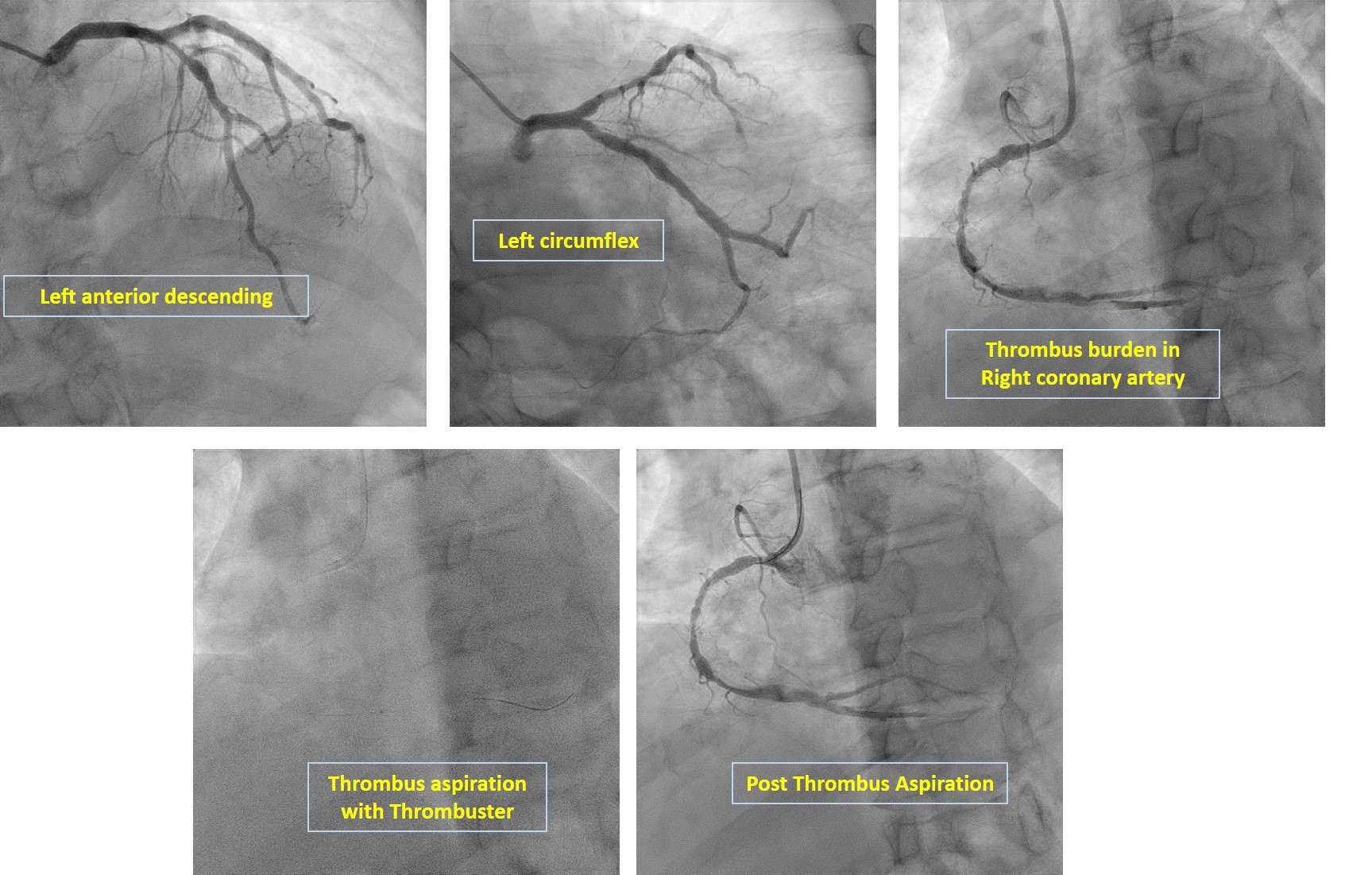
Coronary angiography showed normal left main stem. There was moderate stenosis at the proximal left anterior descending artery (LAD) with ectatic segment. The left circumflex artery (LCX) was ectatic with mild irregularities at the mid segment. The right coronary artery (RCA) had severe stenosis from proximal to mid segment, ectatic distal segment with heavy thrombus burden of grade 4 and TIMI II flow.
 |
|
|
[Interventional Management]
- Procedural step:
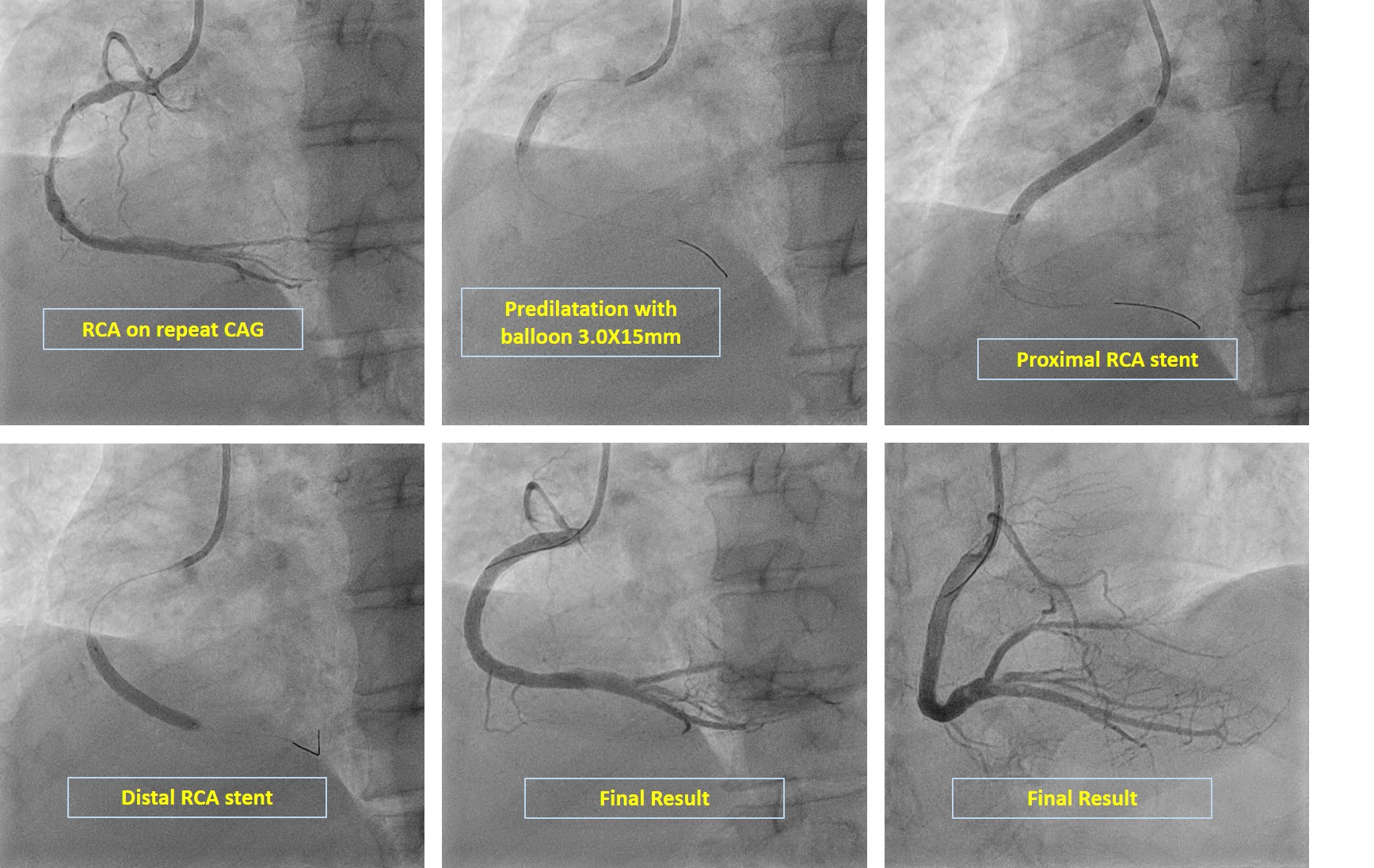
Primary PCI was undergone to the RCA in which guiding catheter JR 3.5X16F was inserted and wired with Runthrough Floppy. Thrombus aspiration was done with Thrombuster, which was unable to retrieve much thrombus and there was still heavy thrombus burden post aspiration. The patient was given bolus dose of intracoronary Glycoprotein IIb/IIIa inhibitor (tirofiban) 13ml followed by intravenous infusion of 12ml per hour for 24 hours. In view of high thrombus burden, we decided for deferred stenting.At repeated coronary angiogram three days later, there was soft plague seen at the distal RCA but no more thrombus in vessel. We decided to proceed with PCI to RCA. Runthrough floppy was used to cross the lesion then predilated with semi-compliant Sapphire II Pro 3.0X15mm to RCA. Then, first stent using Zotarolimus eluting Resolute Onyx 3.5X30mm was deployed at the distal-mid region. The proximal RCA region was predilated with stent balloon followed by ostial to proximal region deployment with Resolute Onyx 4.0X38mm.Subsequently, the overlap area was postdilated with stent balloon at 18 ATM. Lastly, the ostial RCA was flared out with high pressure 20 ATM.TIMI III flow was achieved. Patient was discharged well.
 - Case Summary:
Intracoronary thrombus formation is common in patients with STEMI. Although there is still controversial regarding routine aspiration in primary PCI, high thrombus burden is still an important predictor of outcome in STEMI. This is because high thrombus burden has been associated with incidence of distal embolisation and in itself is associated with PCI failure and adverse outcome in STEMI. Current guidelines suggest that while there is limited evidence to recommend routine use of GPIIb/IIIa inhibitors, they may be considered in this event that showed angiographic evidence of heavy thrombus with slow flow like in our patient.
|
|