Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
CASE20191102_002
| CORONARY - Complications | |
| A Surprise Acute Closure of Wide-Angle Left Circumflex Side Branch During Left Main PCI | |
| Chu Zhen Quek1, Doreen Sumpat2, Heng Shee Kim1, Kim Fong Ng1, Hou Tee Lu1, Benjamin Leo Cheang Leng3, Chuey Yan Lee4 | |
| Sultanah Aminah Hospital, Malaysia1, Universiti Malaysia Sabah, Malaysia2, Columbia Asia Hospital Tebrau, Malaysia3, Hospital Sultanah Aminah, Malaysia4, | |
|
[Clinical Information]
- Patient initials or identifier number:
MNI
-Relevant clinical history and physical exam:
Mr. MNI was a 47 years old gentleman with dyslipidemia. He was a former heavy smoker. He had history of anterior ST Elevation MI 1 month ago during which he received Intravenous Thrombolysis therapy. He did not have family history of coronary vascular diseases. He had CCS class II and NYHA Class II symptoms. His BP was 132/70mmHg. He had unremarkable physical examination findings.
-Relevant test results prior to catheterization:
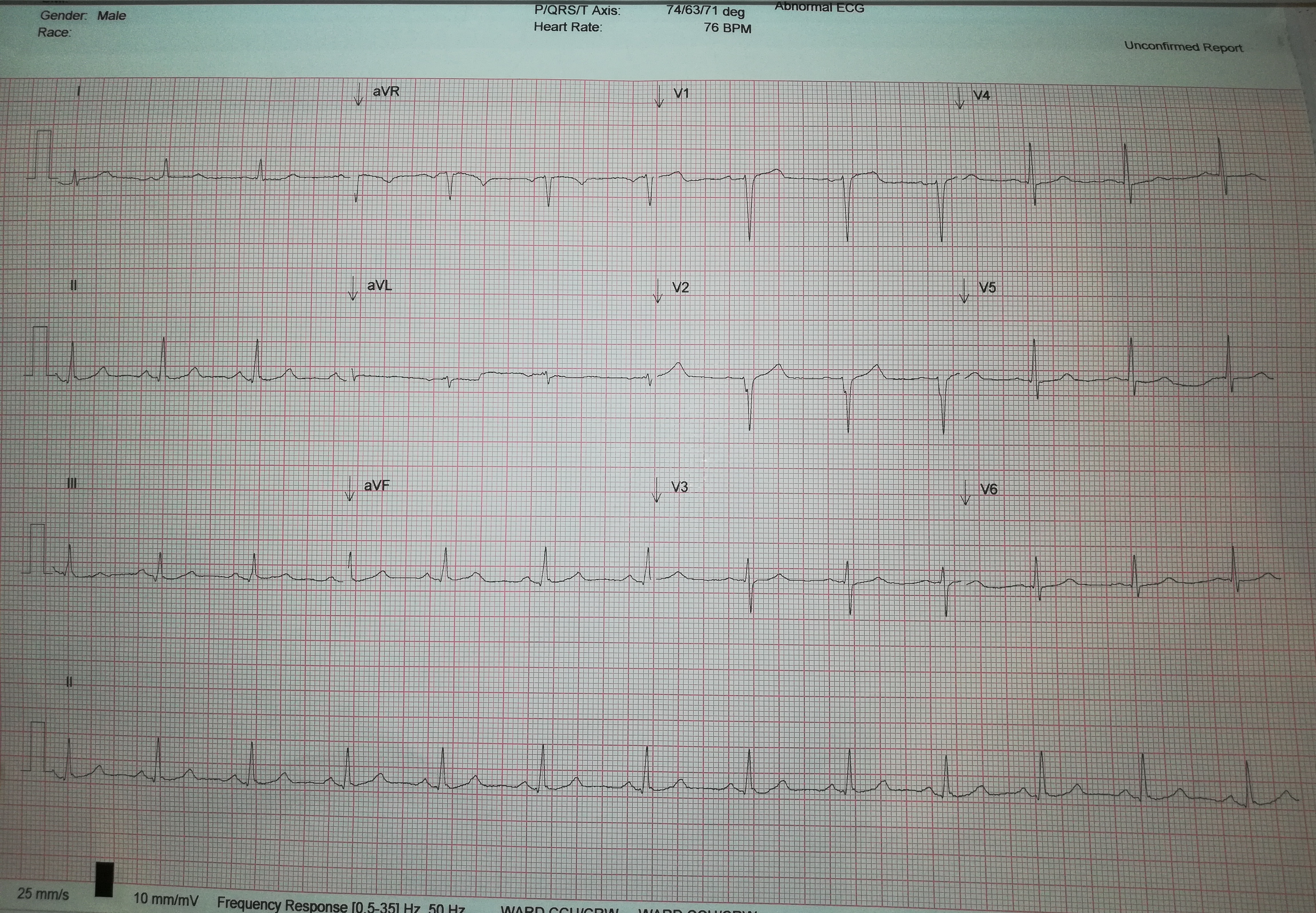
His LVEF was 45-50% with anteroseptal wall hypokinesia. He had inconclusive EST as he could not perform beyond stage II of Bruce protocol. His creatinine was 92mmol/dL. ECG showed pathological 'Q' wave in lead V2.
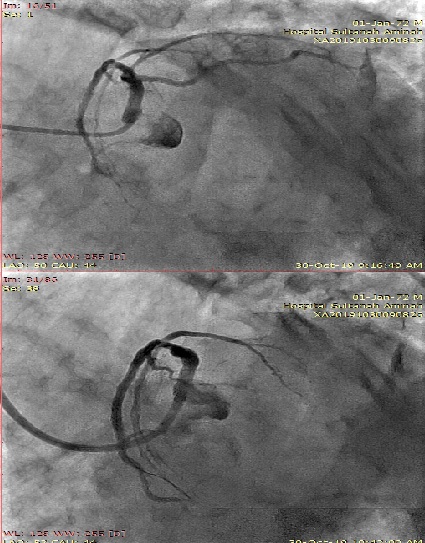
 - Relevant catheterization findings:
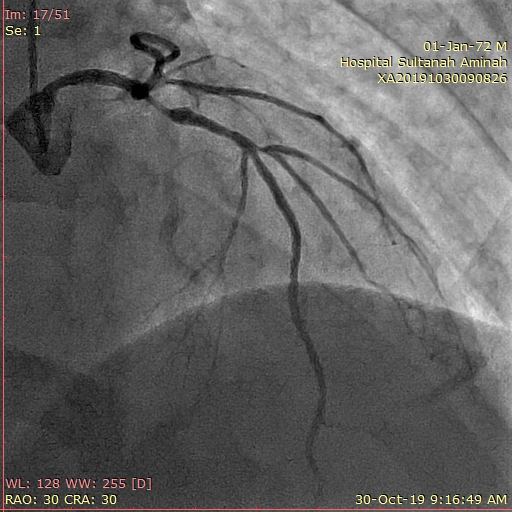
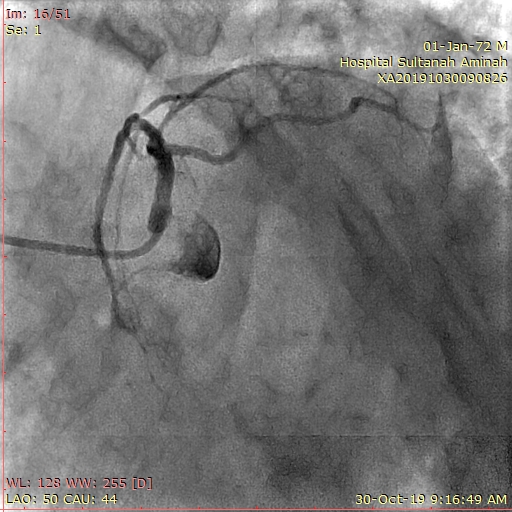
Tandem lesions with Ostial LAD severe stenosis and pLAD borderline stenosis. Ostial LM mild stenosis with no BP dampening with catheter engagement. LCX was recessive with lesion-free and it had 90 degrees take off angle from LAD. LM bifurcation Medina Classification (1-0-0). RCA was dominant and was disease free.
  |
|
|
[Interventional Management]
- Procedural step:
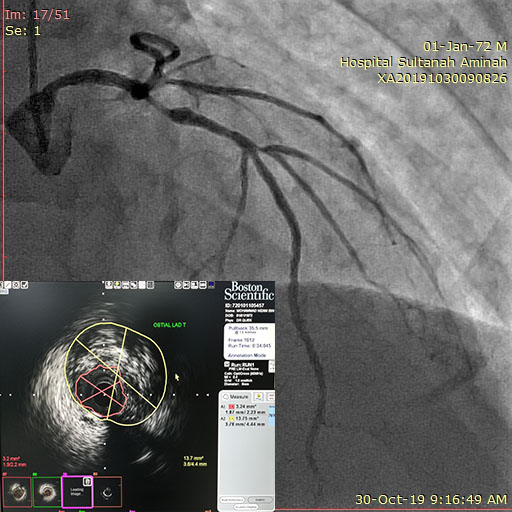
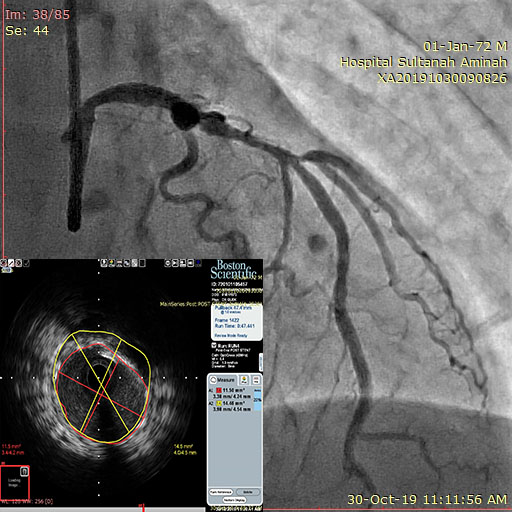
7Fr XB 3.0 Guiding catheter via right femoral artery with 100units/kg IA Heparin administered prior procedure. PT2 PTCA wire advance smoothly into dLAD. There was difficulty to wire the LCX at first as it took off at 90 degrees angle from LM. The ostial LAD lesion was predilated with SCOREFLEX 2.5x15mm Scoring balloon up to 16atm (2.5mm). IVUS showed ostial LAD 4.5mm with fibrous plaque and LM 4.7mm in diameter with disease free at body of LM. pLAD had size discrepancy but acceptable MLA. The strategy was therefore a single crossover stent from body LM to LAD rather than 2 overlapping stent extending to pLAD. Xience Xpedition 4.0x18mm DES deployed up to 12atm (~4.0mm). The stent was postdilated with 4.5x8mm NC balloon up to 20atm with jailed LCX side branch wire. IVUS showed suboptimal MSA at target lesion therefore further postdilatation was needed but it was decided to remove the jailed SB wire. The same 4.5x8mm NC balloon was used to post dilate the target lesion up to 26atm. Now, there was ST elevation at lateral leads with acute closure of LCX. Attempt to wire the LCX at its challenging take-off angle and through the stent strut was unsuccessful. Eventually the LCX spontaneously re-establish flow. In view of difficult wiring it was decided for another staged procedure for SB intervention followed by FKB.
   - Case Summary:
In this case, the LCX side branch was traditionally thought to be safe during bifurcation PCI due to two favoring characteristics i.e. wide-angle take off from LM and disease-free at ostial LCX. Surprisingly it acutely closed after POT which could result from MB plaque shift. Rewiring back the SB after stenting at this wide angle could be technically challenging. Utilization of double-lumen microcatheter with reverse wiring technique could be the solution during bail out of the SB closure. Alternatively, Jailed stent balloon technique could preserve the SB luminal patency during stenting and thus prevent acute SB closure.
|
|