Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
CASE20191028_014
| ENDOVASCULAR - Aorta Disease and Intervention | |
| "Dealing with Luminal Disasters": Catheter Intervention of Resistant Hypertension and Recurrent Pulmonary Edema | |
| Khin Maung Zan Mohd Saad Jalaluddin1 | |
| Hospital Pusrawi, Malaysia1, | |
|
[Clinical Information]
- Patient initials or identifier number:
Mr. NMN
-Relevant clinical history and physical exam:
We describe a 62 year old male with underlying hypertension, dyslipidemia, pervious history of ischemic stroke and CKD stage 3. He presented with recurrent episodes of pulmonary edema and resistant hypertension with systolic blood pressure >200 mmHg despite on 7 anti-hypertensive medications. He was also treated for NSTEMI during recent admission. There was presence of renal bruit and bibasal crackles of lungs. Other physical examinations were unremarkable.
-Relevant test results prior to catheterization:
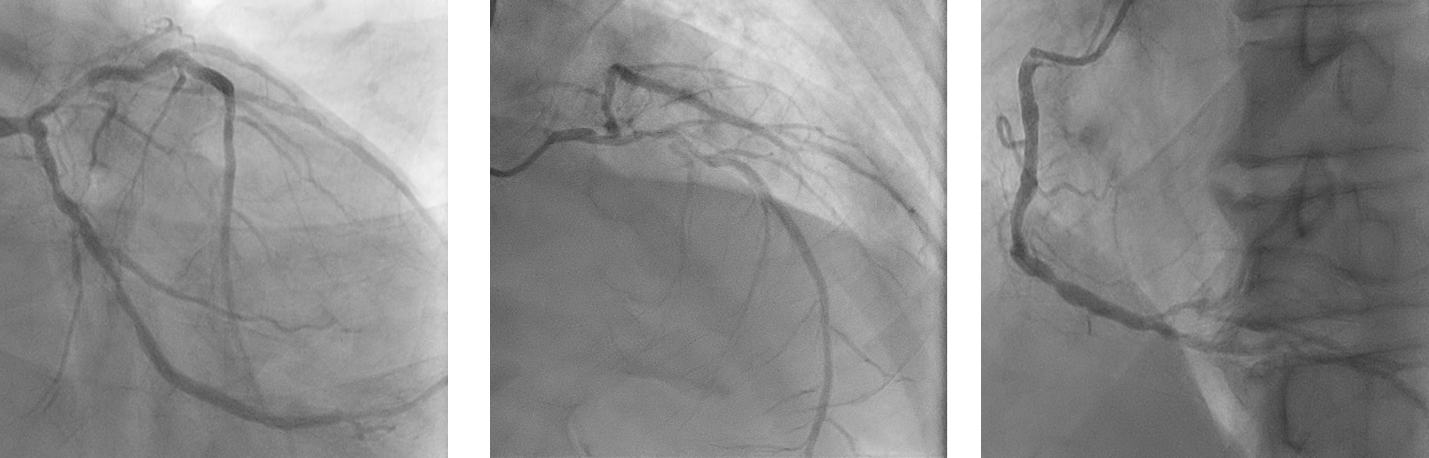
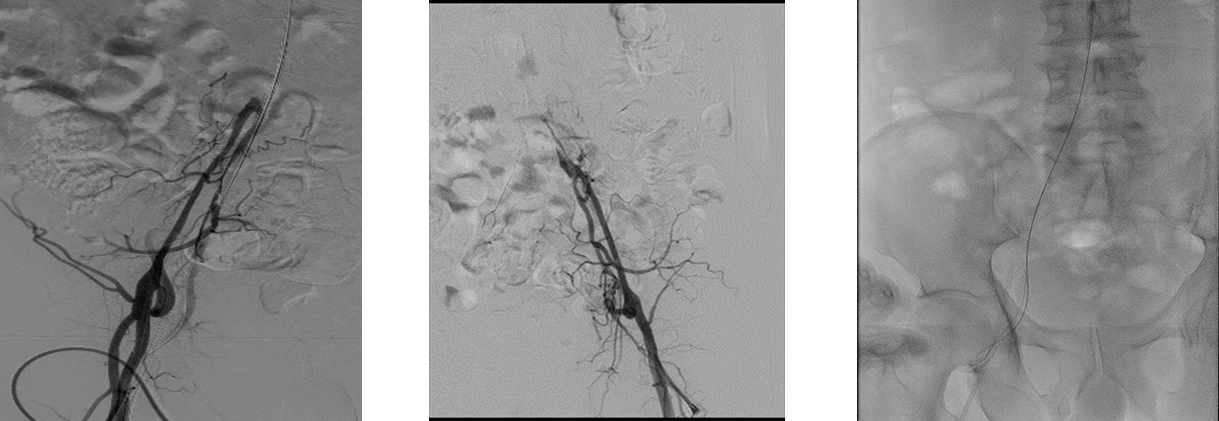
Electrocardiogram showed extensive ST segment depression and T wave inversion with features of LVH and elevated cardiac enzymes. His eGFR was 49 ml/min with normal liver function test and full blood count. Echocardiogram showed LVEF 53% with concentric LVH and normal valves. CT angiogram showed complete occlusion abdominal aorta after superior mesentric artery (SMA) with reconstitution of right and left external iliac arteries via collaterals.  - Relevant catheterization findings:
Coronary angiogram showed moderate disease of distal LMS, severe stenosis of mid LCX, severe stenosis of proximal LAD and severe disease of posterolateral branch of RCA. In view of these findings, we referred him for CABG but surgeon declined due to resistant hypertension. He was then referred to vascular surgeon for bilateral aorto-iliac bypass but was turned down. We proceeded with Percutaneous Transluminal Angioplasty (PTA) of aorto-iliac, hoping that it will bring down the blood pressure.
  |
|
|
[Interventional Management]
- Procedural step:
We proceeded with Percutaneous Transluminal Angioplasty (PTA) of aorto-iliac with left brachial, right and left femoral artery punctures with 6FR sheaths. Attempted to cross with Terumo stiff wire and JR 3.5 6FR antegradely but wire was in the false lumen. Changed to retrograde approach via right femoral access and crossed with command 0.014 wire using SAFARI technique and wire externalized. Predilated and stented infra SMA into right external iliac and right common femoral artery with EPIC 14X60X7.0mm, ABSOLUTE PRO LL7.0X150mm and VASCUFLEX 7.0X80mm. We achieved good flow to right femoral artery but failed to cross left common iliac artery.
His blood pressure came down to 150/90 mmHg soon after the procedure and managed to reduce number of antihypertensives to 4 from 7. He had NSTEMI in the ward with dynamic ECG changes and dropped in LVEF to 38% from 53%. We proceeded with high risk PCI to LM-LAD and LCX. PCI to LCX was done via right radial artery approach with 6FR sheath. Lesion was pre-dilated with 2.5X15 balloon and stented with DES 3.0x19 mm. It was post dilated with NC balloon 3.0x12 mm at 24 atm. PCI to LAD with provisional single stent technique. Pre-dilated the lesion with NC 3.0x12mm and NSE Alpha 3.5x13mm. We were unable to deliver the long DES due to calcified and tortuous proximal LAD. We stented with DES 3.5x18mm and 3.5x26mm. It was post dilated with NC balloon 4.0x8mm at 20 atm. IVUS was done and result accepted. 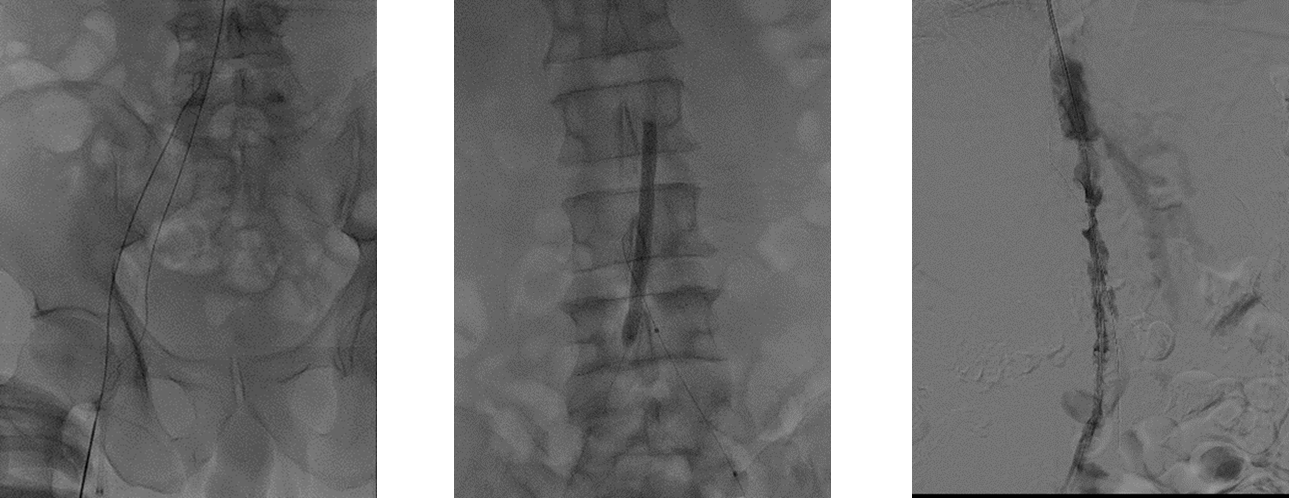 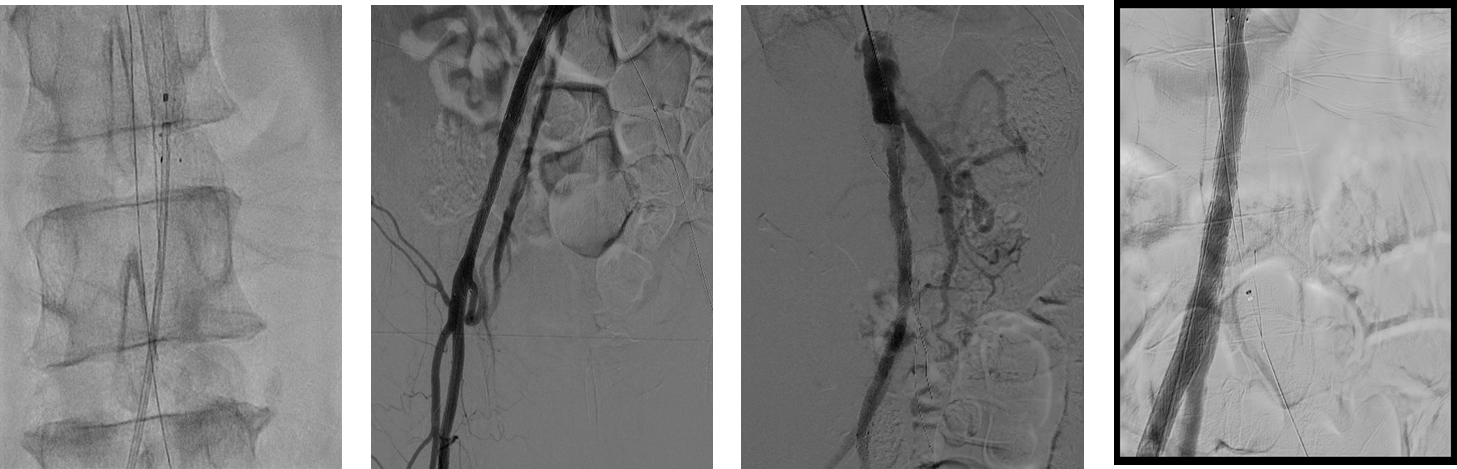 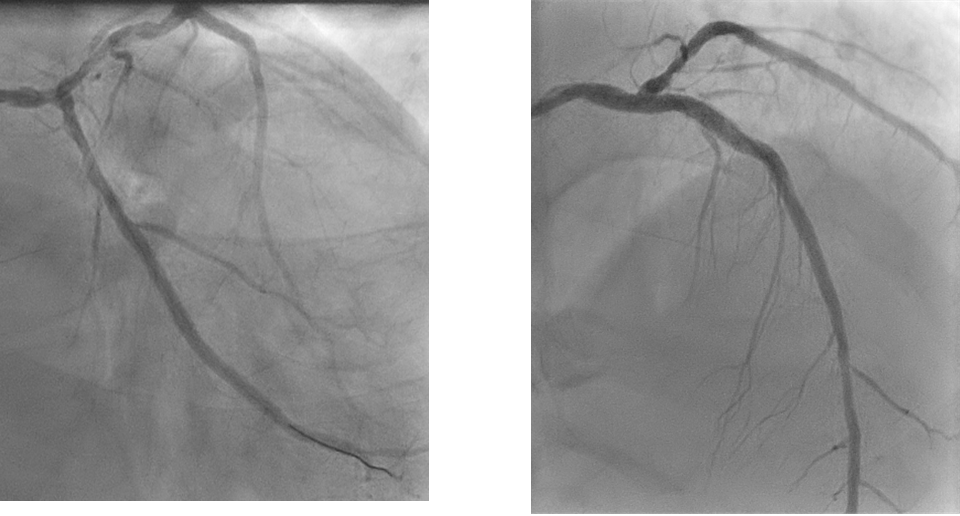 - Case Summary:
We successfully managed to treat refractory hypertension and recurrent pulmonary edema through catheter intervention. We proceeded with peripheral intervention first in order to bring down the blood pressure prior to coronary intervention. Blood pressure control was essential to reduce the risk of haemorrhagic stroke during angioplasty. Patient was able to discharged well 3 days after the procedure. During subsequent follow up, he was asymptomatic with stable blood pressure and improvement of LVEF to 50%.
|
|