Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
CASE20191027_003
| CORONARY - Complex and Higher Risk Procedures for Indicated Patients (CHIP) | |
| The Challenge of Treating an Octogenarian with Left Main Disease and Heavily-Calcified Left Anterior Descending Artery Presented with NSTEMI and Complete Heart Block | |
| Hou Tee Lu1, Chu Zhen Quek1, Heng Shee Kim1, Kim Fong Ng1, Chuey Yan Lee2 | |
| Sultanah Aminah Hospital, Malaysia1, Hospital Sultanah Aminah, Malaysia2, | |
|
[Clinical Information]
- Patient initials or identifier number:
LYL
-Relevant clinical history and physical exam:
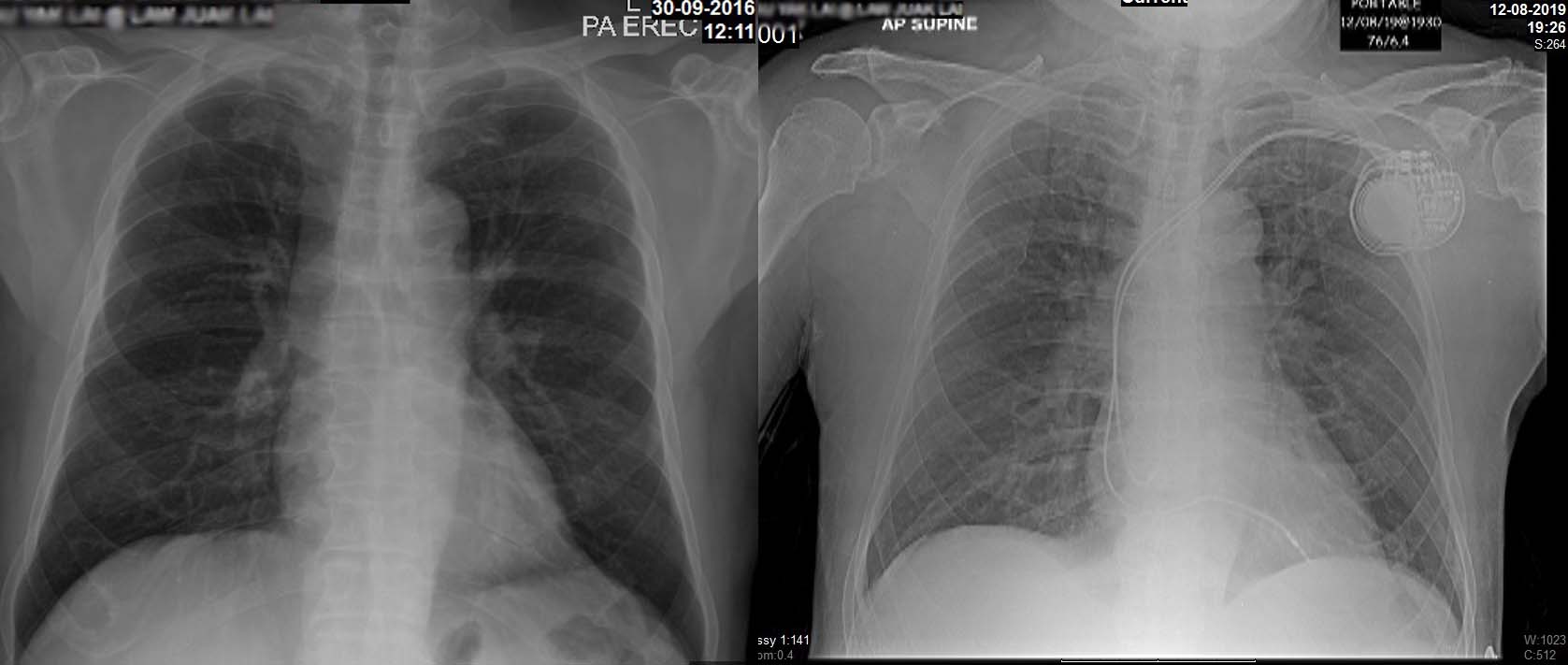
An 86-year-old male complained of chest pain (CCS class III) and dizzy spell for 3 days. He was admitted via A&E. His coronary risk factors included pre-existing ischemic heart disease, diabetes mellitus, hypertension and active smoking. The heart rate was 40/min and blood pressure (BP) was 150/80 mmHg. Clinically, he had symptomatic bradycardia. He's not in heart failure.
-Relevant test results prior to catheterization:
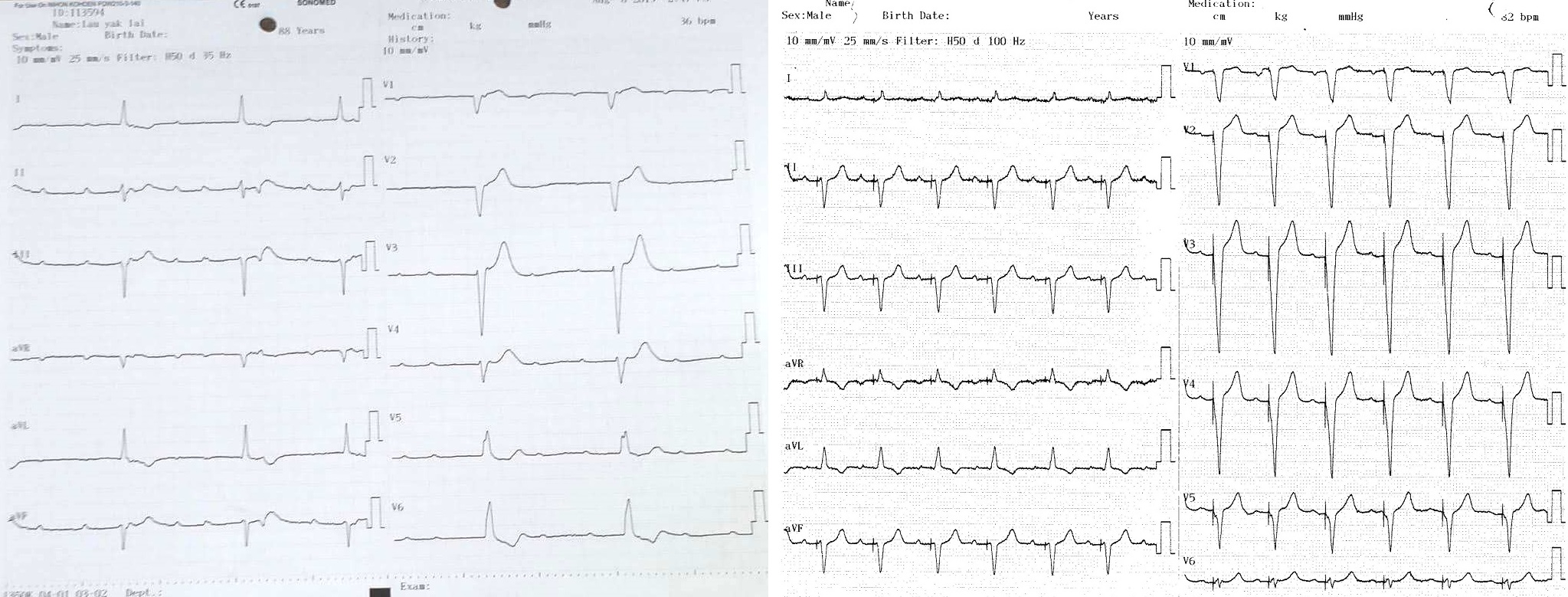
ECG showed complete heart block (CHB). Troponin T was positive. Blood investigations: Hb: 13.3 g/dL, Na: 143 mmol/l, K: 3.9 mmol/l, creatinine: 103 µmol/L, total cholesterol: 6.3 mmol/L and LDL: 3.1 mmol/L, and RBS 7.8 mmol/l. The echocardiography showed EF of 66%. hypokinetic anteroseptal wall. Normal valves and chambers size.
  - Relevant catheterization findings:
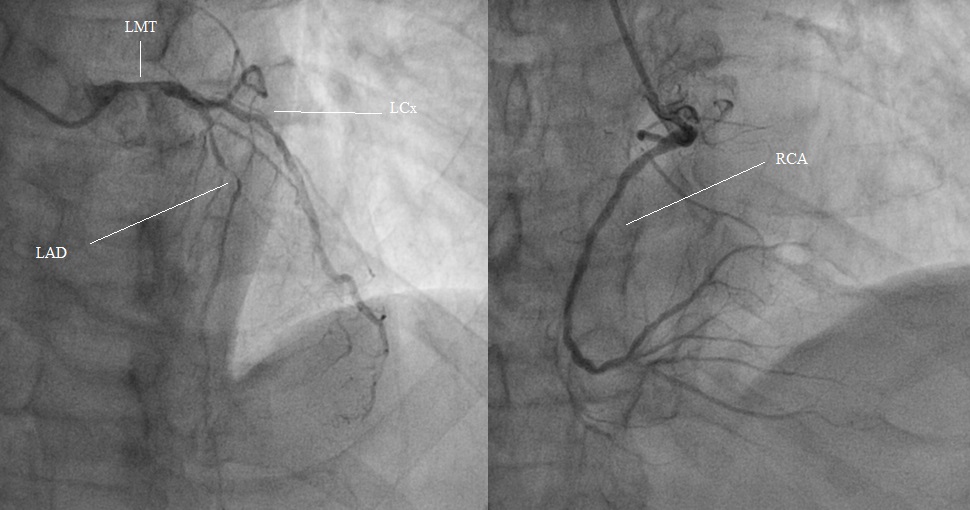
A temporary pacemaker was inserted via RFV. Transradial angiogram:1. LMT, moderately calcified 70% stenosis2. Prox-to-mid LAD artery diffuse, heavily calcified, 95% stenosis3. Mid LCX 50-60% stenosis 4. RCA moderately calcified, 30% stenosisSYNTAX score: 32 STS score: Mortality: 3.9 %, morbidity and mortality: 23%Patient was referred for CABG but declined because of old age. We implanted a pacemaker for the irreversible CHB before PCI. No major bleeding.
|
|
|
[Interventional Management]
- Procedural step:
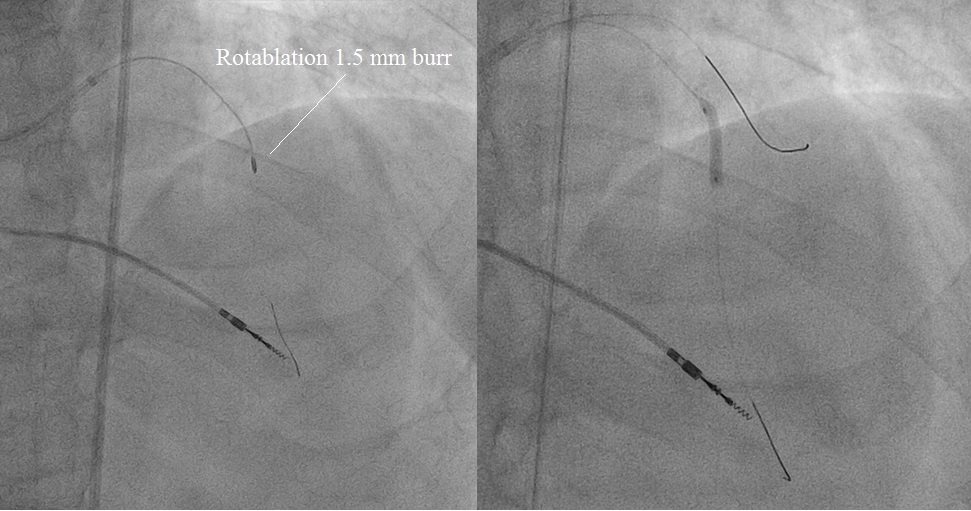
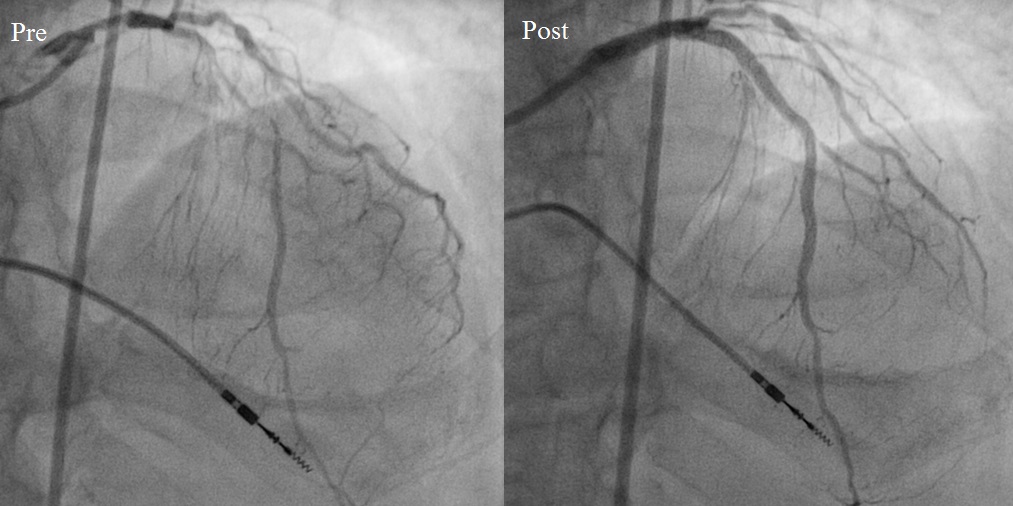
Right and left femoral arteries punctured. IABP was on standby mode. A 7Fr EBU 3.5 was used to engage LMT. IVUS was performed to assess LMT, proximal LAD and LCX. A SION wire was wired into LAD and exchanged with a floppy Rotawire via a microcatheter. Rotational atherectomy (1.5 mm burr) was done on LMT and LAD. After successful Rotablation, balloon angioplasty was performed using NC EMERGE 2.0x12mm, 2.5x15mm balloons. IVUS examination was performed after balloon angioplasty. The LAD lesion was treated with SYNERGY 2.5x48 mm. Ostial LMT to proximal LAD was treated with PROMUS 4.0x24mm. Repeat IVUS. Mid LCX was treated with drug-eluting balloon (Sequent Please) 2.5x15mm balloon. The LMT-LAD-LCX bifurcation lesion was treated by kissing balloon technique (KBT). Final kissing balloon was done: LMT-LAD: NC EMERGE 4.0x12mm, LMT-LCX: NC EMERGE 3.5x15mm. Finally, POT was performed on LM stent with NC EMERGE 4.0x12mm balloon at high pressure. Final IVUS showed good apposition and well-expanded stents. Patient had good functional recovery at 1 month follow-up.
   - Case Summary:
IVUS-guided PCI with Rotational artherectomy should be considered as an alternative intervention strategy in elderly high-risk patient with left main disease and heavily-calcified lesions when CABG is not feasible. Treating the complete heart block by a dual chamber pacemaker prior to PCI is safe and may de-escalate the risk of PCI.
|
|