Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
CASE20191016_002
| CORONARY - Complex and Higher Risk Procedures for Indicated Patients (CHIP) | |
| Severely Calcified Three-Vessel Coronary Disease with Ischemic Cardiomyopathy and End Stage Renal Failure in a Poor Surgical Candidate Treated Successfully by PCI and Rotational Atherectomy | |
| Kim Fong Ng1, Chu Zhen Quek1, Heng Shee Kim1, Chuey Yan Lee2, Hou Tee Lu1 | |
| Sultanah Aminah Hospital, Malaysia1, Hospital Sultanah Aminah, Malaysia2, | |
|
[Clinical Information]
- Patient initials or identifier number:
CYM
-Relevant clinical history and physical exam:
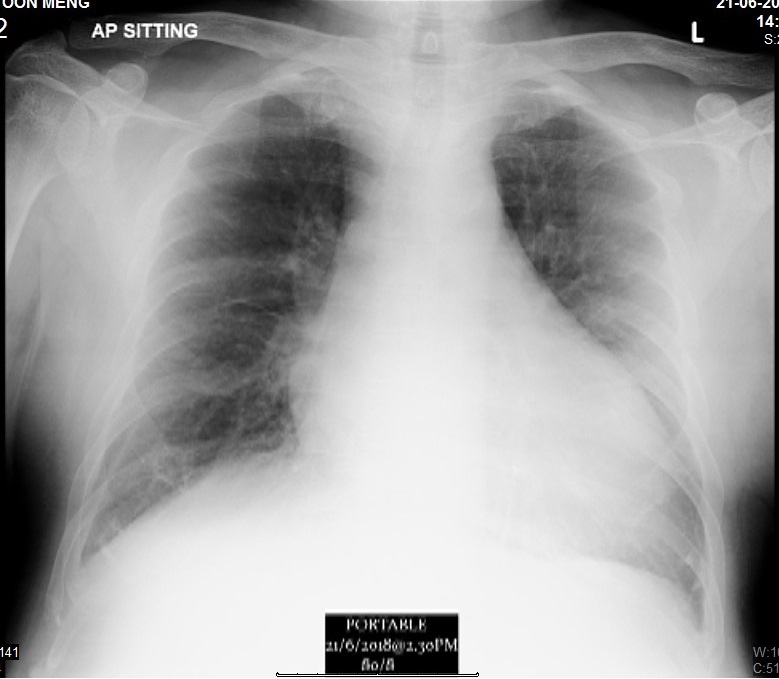
A 56-year-old male was referred by a nephrologist for disabling angina during hemodialysis. Hemodialysis was interrupted due to low BP. He had frequent admissions to a district hospital for unstable angina. Past medical history included end stage renal failure (ESRF), diabetes mellitus, and hypertension. Non-smoker. The heart rate was 95/min and BP was 100/50 mmHg. Lungs had bilateral pulmonary edema and pedal edema was noted during admission.
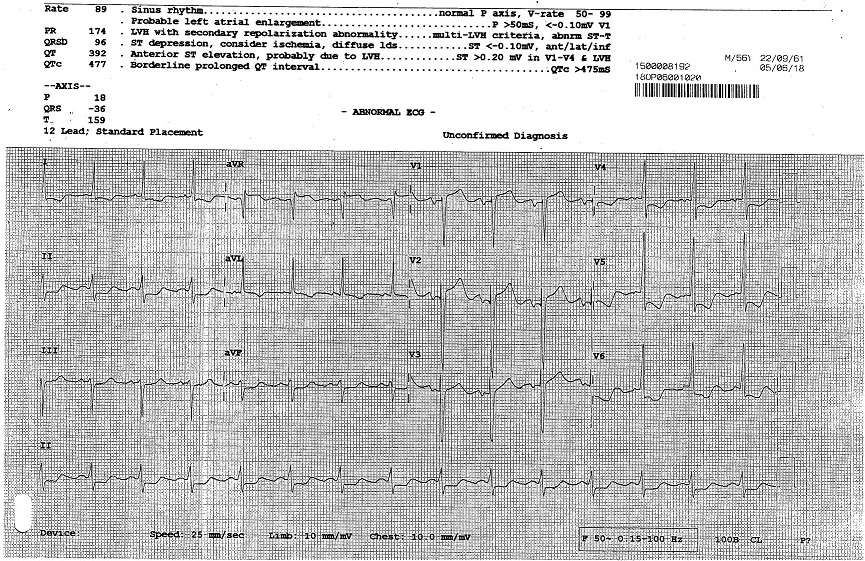 -Relevant test results prior to catheterization:
ECG showed horizontal ST depression at V3-6. Troponin T was positive (1867 ng/L). Blood investigations: Hb: 11.4 g/dL, creatinine: 658 µmol/L, total cholesterol: 3.1 mmol/L and LDL: 1.7 mmol/L, and RBS 6.5 mmol/l. The echocardiography showed impaired EF of 30%. Dilated left ventricle. Globally hypokinetic left ventricular wall. Normal valves.
 - Relevant catheterization findings:
Coronary Angiography1. LMT normal 2. LAD artery 80% stenosis, moderately calcified proximal to mid LAD, diffuse small vessel disease3. LCX artery 90% stenosis, heavily calcified4. RCA mid heavily calcified 70%, distal 95% stenosis
Referred for high risk CABG. Surgical turned down due to poor target for graft, heart failure, ESRF and recent NSTEMI. Patient was scheduled for high risk PCI after Heart Team discussion. High risk consent was obtained. |
|
|
[Interventional Management]
- Procedural step:
First procedure (LAD): The right femoral artery (RFA) was punctured. IABP was on standby mode. A 6Fr EBU 3.5 was used to engage LMT. The LAD was predilated by NC 2.0x8mm balloon. Long LAD lesions was treated with paclitaxel-eluting balloons (PEB) (2.0x20mm, 2.0x20mm, 2.0x25mm). Patient was stable after first index PCI. He was schedule for second PCI one month later. Second procedure (LCX): RFA approach. EBU 3.5, 7Fr. A PT2 wire was inserted in LCX and exchanged with a floppy Rotawire via a micro catheter. Rotational atherectomy (RA) (1.75 mm burr) was done. Balloon angioplasty was done using a 3.0x15mm NC balloon. The mid LCX lesion was treated with EES 3.0x38mm. Proximal LCX was treated with PEB (3.0x25mm). Good result. Third procedure (RCA): A month later. RCA was engaged with JR 4.0, 7Fr. The repeat angiogram showed good angiographic result of the LAD and LCX. The RCA lesion was treated successfully by RA (1.5 mm burr) and drug-eluting stents (EES, 3.5x32mm, 3.0x28mm).
Patient underwent hemodialysis well after the second index procedure. His functional status improved remarkably after revascularization. 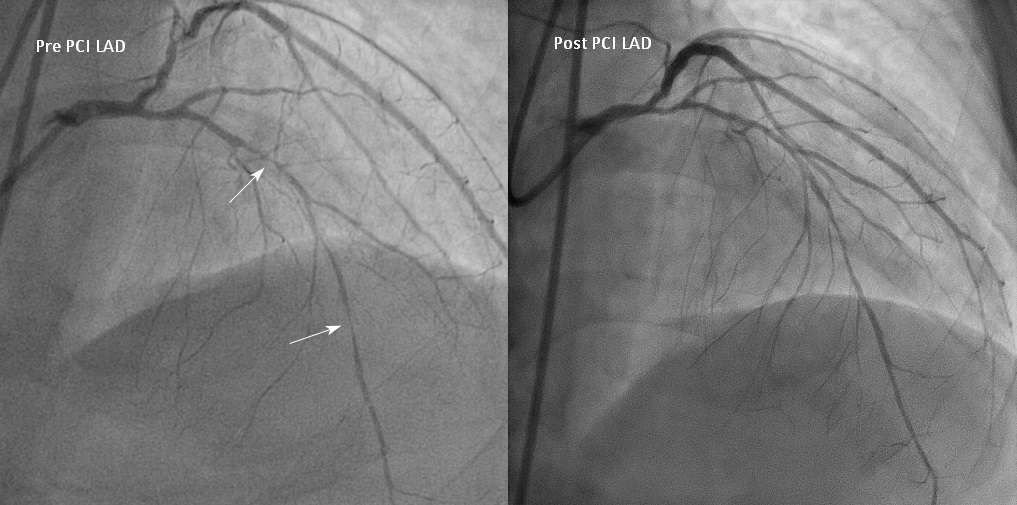 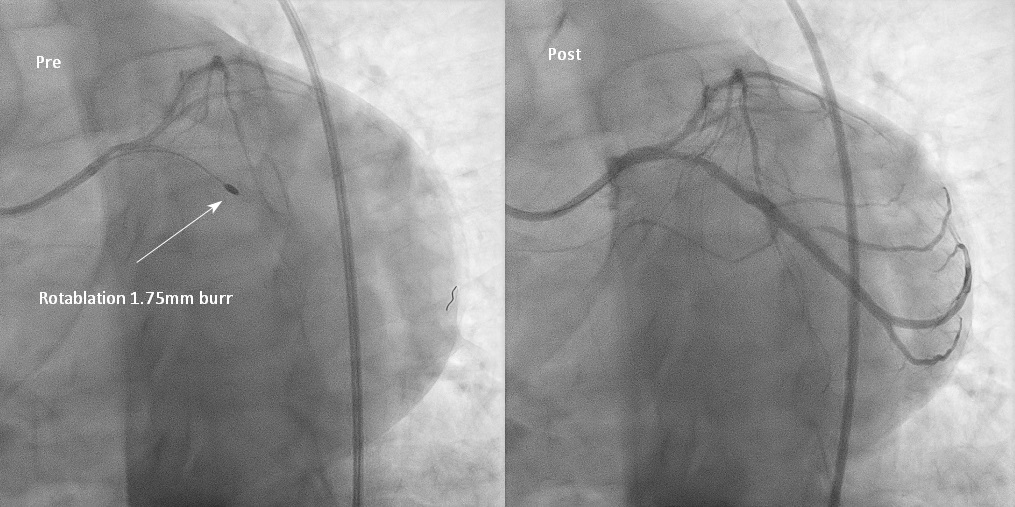 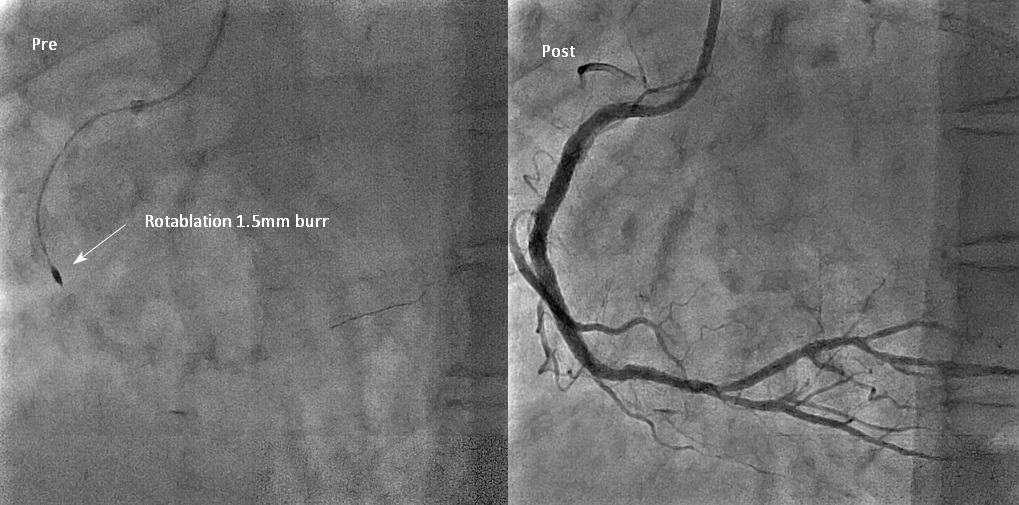 - Case Summary:
In patient with diabetes, CABG should be the preferred strategy for multivessel revascularization. However, CABG may not be feasible in certain high-risk patients. Our case demonstrated that in a patient with ESRF, recent MI and heart failure, PCI using Rotational atherectomy and drug-eluting stent to treat a complex, heavily calcified three-vessel disease is feasible with favorable outcome and low complication rate.
|
|