Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
CASE20191014_002
| CORONARY - Acute Coronary Syndromes (STEMI, NSTE-ACS) | |
| Discovering the Right Path Is Not Always Easy. | |
| Chan Ho Thum1 | |
| National Heart Institute, Malaysia1, | |
|
[Clinical Information]
- Patient initials or identifier number:
DMRBMA
-Relevant clinical history and physical exam:
We present a 38 year old medical practitioner with no underlying medical co-morbids. He presented with sudden onset of epigastric discomfort with associated giddiness, diaphoresis and vomitting. Blood pressure was stable but he was bradycardic at 40 beats per minute requiring intravenous atropine. Physical examination was unremarkable. He was a smoker.
-Relevant test results prior to catheterization:
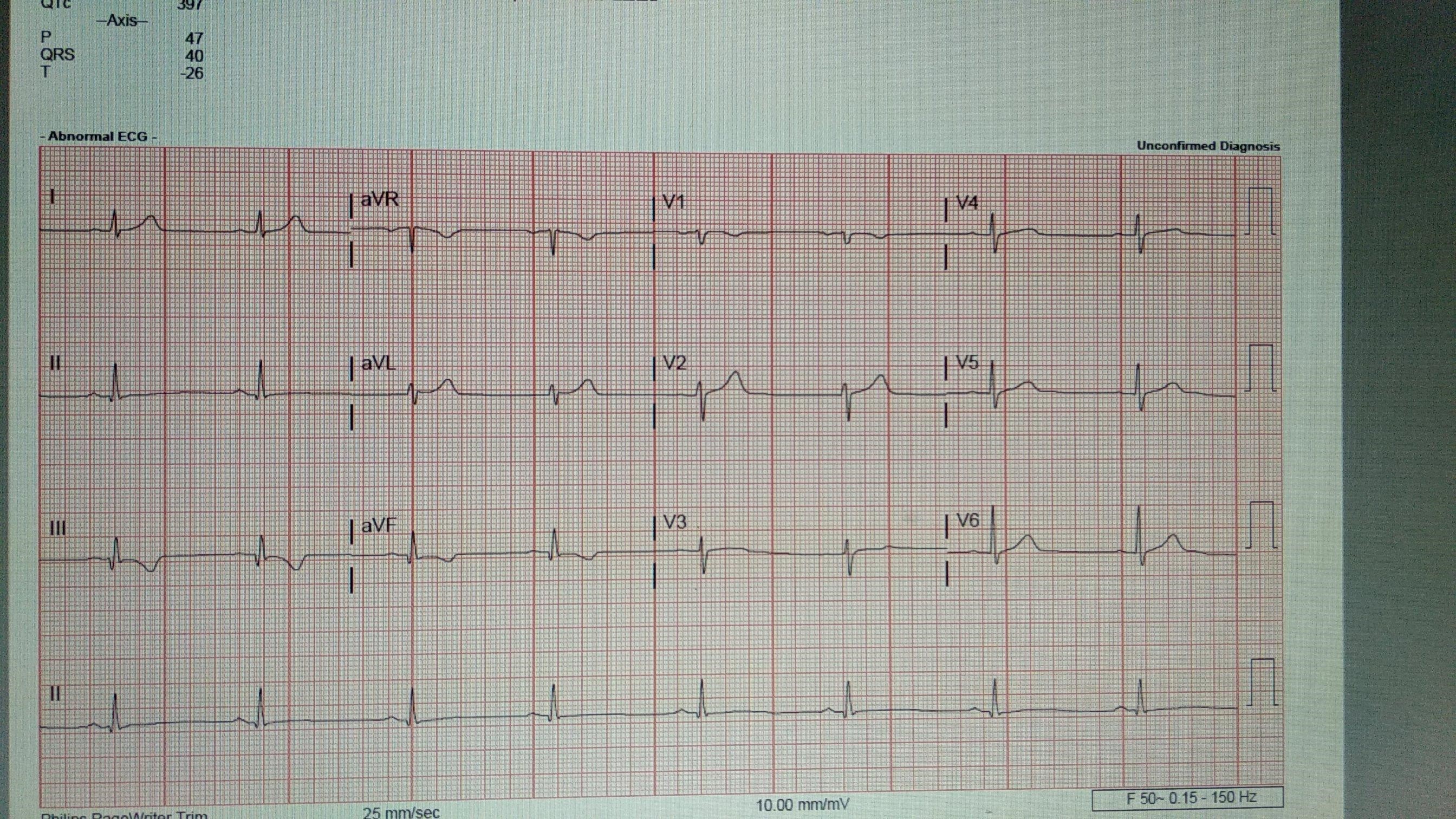
Urgent ECG revealed Q waves and T inversion on his inferior leads. Troponin T was 3131 pg/ml. Bedside echo revealed inferior wall hypokinesia. He was diagnosed with Non ST elevation myocardial infarction and we proceeded with an urgent coronary angiogram for him.
 - Relevant catheterization findings:
Coronary angiogram via right radial approach showed a normal left main artery, a moderate diseased mid left anterior descending artery and a normal circumflex artery with collaterals and retrograde flow seen to the right side. After much difficulty, we discovered a proximal chronic total occlusion of an anomalous right coronary artery originating from the left coronary sinus.
|
|
|
[Interventional Management]
- Procedural step:
We converted to a femoral approach for better stability. Attempts to wire down the RCA with JR 3.5/6F guiding catheter followed by the XB 6F catheter failed due to guide instability. We decided to stage the procedure in view of prolonged time and high volume of contrast used. During the staged PCI, we successfully engaged the RCA with JL4.0/6Fr guiding catheter. Fortunately for the patient, the RCA had some recanalization revealing severe narrowing of the proximal RCA which we successfully wired through. IVUS done showed a large (5.0mm) Proximal RCA without thrombus.We had to engage the guiding catheter deeper to stabilize the system prior to predilation with 3.5/15mm compliant balloon and 4.0/13mm cutting balloon.The guide became unstable after predilatation, making stent deployment impossible. AL and XB catheter utilized were also unsuccessful. Finally, we tried again to use JR 3.5/6F catheter (which was the initial failed guiding catheter used prior to the staged PCI). This time however, we paired the catheter with the buddy wire technique and this managed to stabilise the system. We successfully stented the lesion with 4.5/18 mm drug eluting stent at 12 ATM. Under IVUS guidance, we post dilated the stent with NC balloon 5.0/15 mm at 18 ATM.
We successfully re-establish TIMI 3 flow back to the RCA with anomalous origin. - Case Summary:
Patients with anomalous RCA may rarely present with acute coronary syndromes. Although challenging, coronary intervention is still feasible, keeping in mind the various guiding catheter and stabilisation techniques available. Stability of the guiding system is the key for procedural success as demonstrated in this case.
|
|