Optical coherence tomography (OCT) was shown in ILUMIEN I to have a profound effect on operator decision-making process during PCI. This study evaluated a standardized OCT workflow on PCI decision making in a real-world population, and assessed impact of physician experience.
Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
ABS20200709_0001
| Imaging: Intravascular | |
| Analysis of Decision-making Process During Optical Coherence Tomography-guided Percutaneous Coronary Interventions – Insights from the LightLab Initiative | |
| Hiram Bezerra1, Luis Augusto Palma Dallan2, Gabriel Tensol Rodrigues Pereira2, Jana Buccola3, Richard Rapoza3, Nick West3, Jason Wollmuth4, John Lopez5, Brian Bergmark6, Kevin Croce6 | |
| Tampa General Hospital, USA1, University Hospitals Cleveland Medical Center, USA2, Abbott Vascular, USA3, Providence St. Vincent, USA4, Loyola University Medical Center, USA5, Brigham and Women¡¯s Hospital, USA6 | |
|
Background:
|
|
|
Methods:
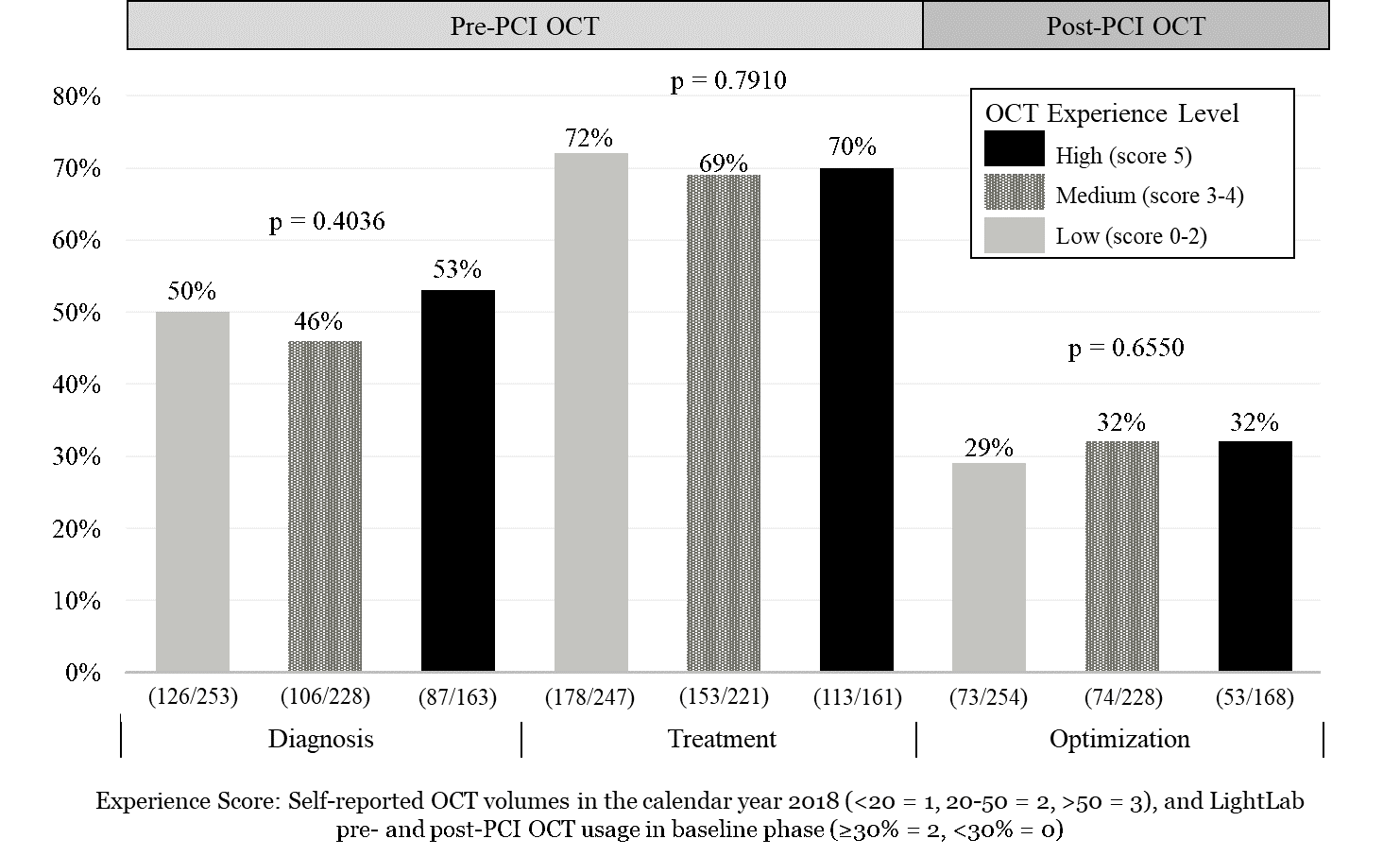
The LightLab Initiative collects real-time, prospective data, on utilization of a prescribed OCT workflow in 4 phases of implementation. In Phase 1, we examined the impact of a standardized OCT workflow on procedural decision making compared with an angiography guided strategy as well as the impact of prior physician OCT experience in the same population. Physicians were stratified according to their expertise with OCT (low, medium and high), based on previous OCT use and experience with prescriptive OCT workflow utilization.
|
|
|
Results:
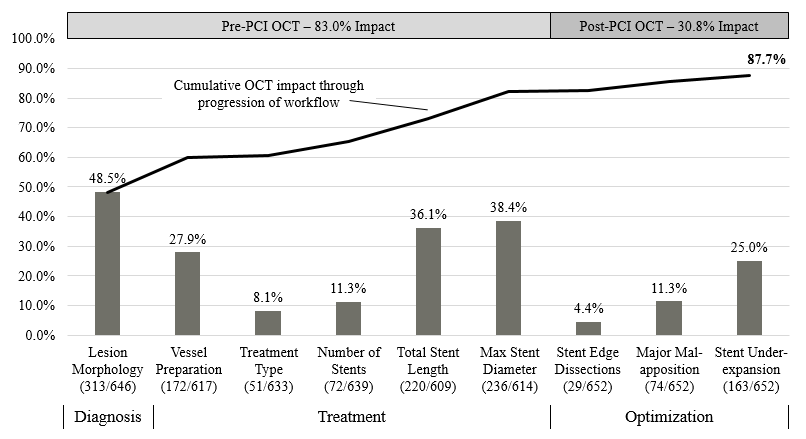
Results for 710 patients who underwent PCI procedures are reported. Of these, 85% (n=604) of cases utilized the prescribed OCT workflow in at least 1 lesion, for a total of 652 (75%) evaluable lesions. Overall, 88% of lesion-level procedural decision-making was impacted with OCT (83% pre-PCI and 31% post-PCI). Compared with angiography alone, pre-PCI OCT resulted in changes in the operator assessment of lesions morphology (48%); treatment type (8.1%); type of vessel preparation (28%), stent diameter (38%), and stent length (36%) (Figure 1). Post-PCI OCT guidance identified underexpansion enabling targeted optimization in 25% of lesions. There was no significant difference in clinical decision making changes in diagnosis, treatment, and optimization among physician experience groups (Figure 2).
  |
|
|
Conclusion:
The LightLab initiative is a unique approach to gathering OCT procedural data, and demonstrates marked impact of OCT on lesion assessment, procedural planning, and stent optimization. Previous experience with OCT does not influence the likelihood of changes to clinical decision making with a prescribed OCT workflow, which suggests that OCT provides novel information for decision making compared with angiography even in experienced users.
|
|