Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
ABS20191115_0023
| Acute Coronary Syndromes (STEMI, NSTE-ACS) | |
| Comparison of 1 Year Composite Events Following ST-Segment Elevation Myocardial Infarction(STEMI) and Non-ST-Segment Elevation Myocardial Infarction(NSTEMI) | |
| Moo Hyun Kim1, XUAN JIN1, Kwang-Min Lee2 | |
| Dong-A University Hospital, Korea (Republic of)1, Dong-A University Medical Center, Korea (Republic of)2 | |
|
Background:
The difference of mortality risk between ST-segment elevation myocardial infarction (STEMI) and non-STEMI (NSTEMI) has not been thoroughly evaluated yet. We sought to compare clinical outcomes of ST-segment Elevation Myocardial Infarction and Non-ST-segment Elevation Myocardial Infarction over 1-years follow-up using Korean Registry of Regional Cardiocerebrovascular center for Acute Myocardial Infarction (KRAMI).
|
|
|
Methods:
From the Korean Registry of Regional Cardiocerebrovascular center for Acute Myocardial Infarction (July 2016 - Sept 2018), patients over 18 years old who underwent acute myocardial infarction were selected. We included patients who had STEMI and NSTEMI and excluded in-hospital mortality. We compared in-hospital death and long-term (within 1-year) mortality, composite in NSTEMI patients with those in STEMI patients.
|
|
|
Results:
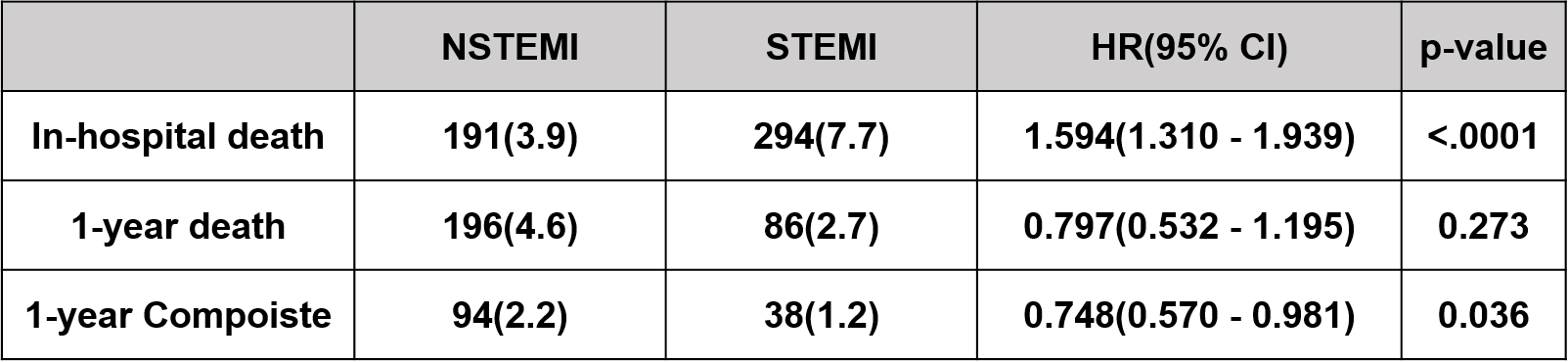
From July 2016 through Sept 2018, a total of 8,733 patients were enrolled at the KRAMI: 3,839 enrolled in the STEMI patients and 4,894 enrolled in the NSTEMI patients. The STEMI patients, as compared with NSTEMI patients, was difference in in-hospital death (HR=11594[1.310-1.939], p=0.000), in 1year composite(HR=0.748[0.570-0.981], p=0.000). (Table 1).
 |
|
|
Conclusion:
The short-term all-cause death events in patients with STEMI were significantly higher than NSTEMI, but the long-term composite events in patients with NSTEMI were significantly higher than STEMI.
|
|