Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
ABS20191115_0001
| Complex and Higher Risk Procedures for Indicated Patients (CHIP) | |
| Long-Term Outcomes of Unprotected Left Main Coronary Artery Disease: Comparison Between Coronary Artery Bypass Grafting and Percutaneous Coronary Intervention | |
| Kai Song1, Moo Hyun Kim2, Jia Xin Li1 | |
| Dong-A University Medical Center, Korea (Republic of)1, Dong-A University Hospital, Korea (Republic of)2 | |
|
Background:
We compared 5 years of outcomes of coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI) for unprotected left main coronary artery (ULMCA) disease in a real-world population. The ideal revascularization strategy for ULMCA disease is unknown. Contemporary randomized trials have reported conflicting results with the two revascularization strategies for the treatment of ULMCA disease at intermediate-term follow-up. An observational study reported similar rates of death and serious composite outcomes but a higher rate of target vessel revascularization with CABG and PCI for ULMCA disease at 5 years. However, PCI with drug-eluting stents had a higher mortality rate compared with CABG.
|
|
|
Methods:
We selected 745 patients with ULMCA disease who underwent CABG (n=479) or PCI(n=266) from 1998-2014. The primary outcome measure was major adverse cardiac and cerebrovascular events (MACCE), defined as the composite of all-cause death, non-fatal myocardial infarction (MI), stroke, or target vessel revascularization (TVR) at 5 years.
|
|
|
Results:
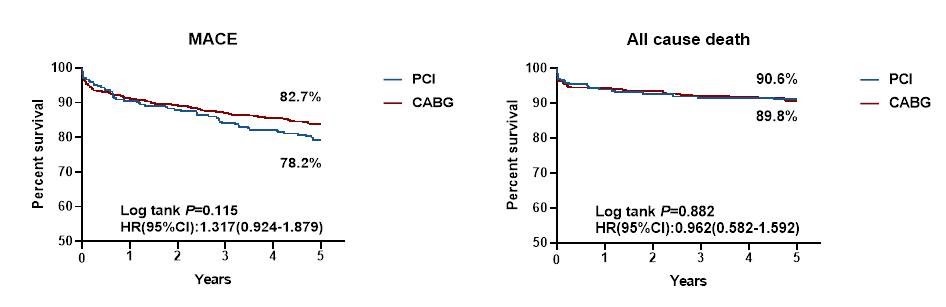
The cumulative 5-year percent survival for MACCE was not significant between the PCI and CABG groups (78.2% vs. 82.7%, log-rank p=0.115). The risk of all-cause death was not significantly different between the 2 groups (log-rank p=0.882). The risk ratio for stroke was not significantly lower with PCI (log-rank p=0.175). The risk ratio for TVR was significantly higher with PCI compared with CABG (log-rank p<0.001).
 |
|
|
Conclusion:
Inpatients with unprotected left main coronary artery disease, PCI was similar to CABG for long-term MACCE, death. The TVR rate was higher in the PCI group.
|
|