Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
ABS20191101_0008
| Complications | |
| Procedural Predictors of No-Reflow Phenomenon After Primary Percutaneous Coronary Intervention in Patients with ST-Elevation Myocardial Infarction | |
| Mahmoud Salem1, Ayman Saeyeldin2, Mahmoud Khalil3 | |
| Lahey Hospital and Medical Center, USA1, Saint Mary's Hospital, USA2, Tanta University Hospital, Egypt3 | |
|
Background:
No-reflow phenomenon (NRP) after percutaneous coronary intervention (PCI) is defined as reduced coronary antegrade flow of thrombolysis in myocardial infarction (TIMI) flow grade ¡Â 2 without mechanical obstruction after recanalization. NRP is associated with poor left ventricle (LV) functional recovery and survival in the early phase of ST-elevation myocardial infarction (STEMI). We sought to evaluate the predictors of NRP following primary PCI.
|
|
|
Methods:
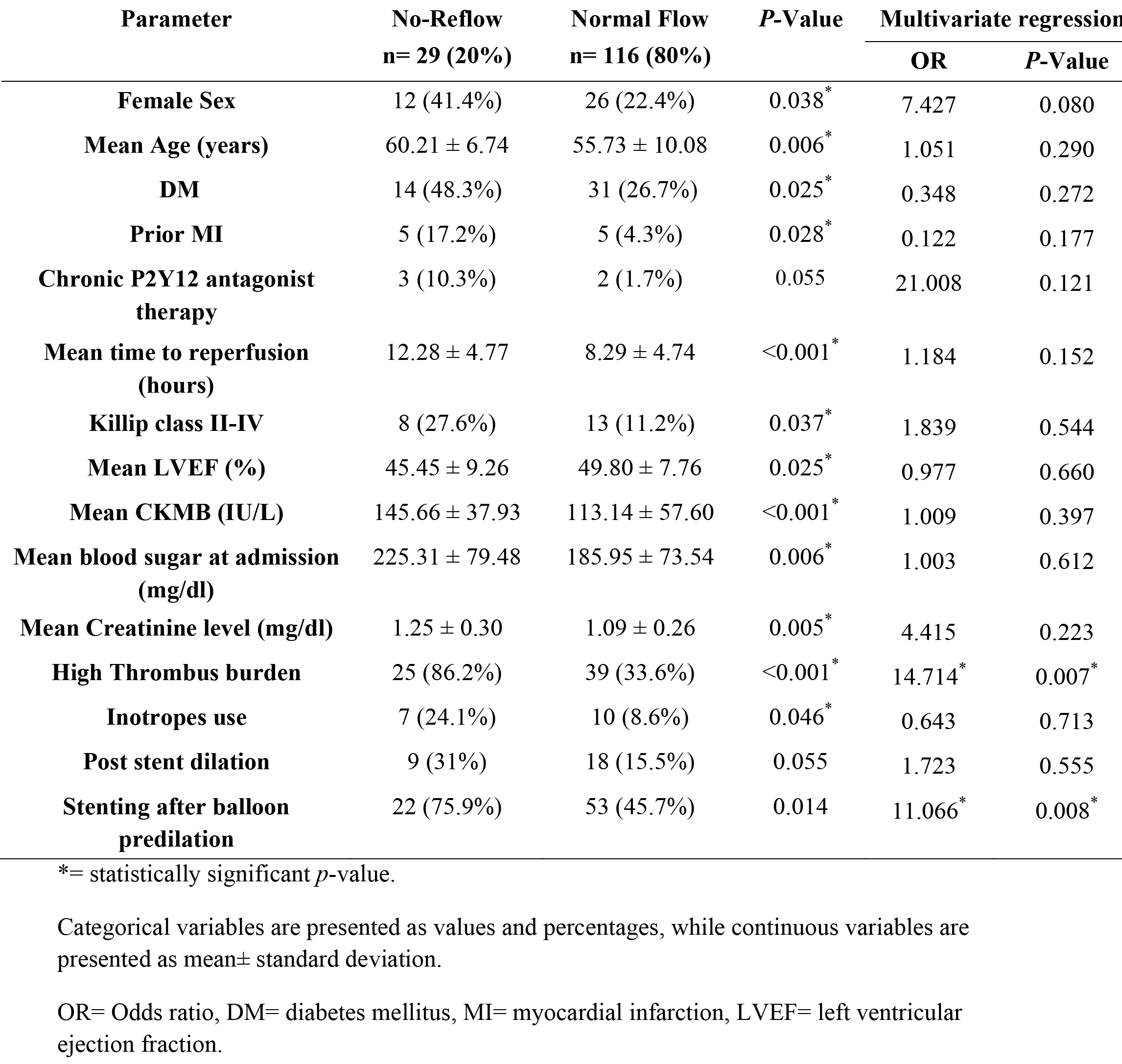
For 6 months, 145 consecutive patients with acute STEMI who underwent primary PCI were followed. Clinical and procedural data were collected for each subject. Patients were divided into two groups: patients with NRP (group I, n = 29) and patients without NRP (group II, n = 116). Multivariable logistic regression was utilized to analyze the predictors of NRP.
|
|
|
Results:
NRP occurred in 29/145 (20%) of patients who underwent PCI. NRP was significantly more frequent in women, patients with increased time to reperfusion, low ejection fraction, high thrombus burden, initial TIMI flow grade 0, and stenting after balloon predilatation (p < 0.05 for all). Logistic regression analysis showed that high thrombus burden (OR: 14.71, p = 0.007) and stenting after balloon predilatation (OR: 11.06, p = 0.008) were independent predictors of NRP. There were no significant differences between the two groups with respect to number of diseased vessels, target lesion location, use of glycoprotein IIb/ IIIa inhibitors, post stent dilation or thrombus aspiration.
 |
|
|
Conclusion:
High thrombus burden and predilatation before stenting (compared to direct stenting) are predictors of NRP after primary PCI in patients presenting with acute STEMI. Thus, direct stenting strategy should be considered when possible.
|
|