Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
ABS20191101_0007
| Chronic Total Occlusion | |
| Clinical Implications of Longer Procedure Time During Chronic Total Occlusion Intervention | |
| Jin-Ho Kim1, Byeong-Keuk Kim2, Chul-Min Ahn, Jung-Sun Kim, Young-Guk Ko, Donghoon Choi, Myeong-Ki Hong, Yangsoo Jang3 | |
| Myongji Hosptial, Korea (Republic of)1, Yonsei University Severance Hospital, Korea (Republic of)2, YONSEI UNIVERSITY COLLEGE OF MEDICINE, Korea (Republic of)3 | |
|
Background:
Although procedure time of chronic total occlusion (CTO) coronary lesion is usually longer than non-CTO lesion, clinical implication for the longer procedure time is not unclear.
|
|
|
Methods:
We enrolled 470 patients who underwent CTO intervention. Longer procedure-time, defined as first quartile of total procedure time in this study, was 112 minutes. We evaluated for acute periprocedural myocardial infarction (PMI), defined as an increase creatine kinase-MB ¡Ã3x the upper limit of normal after intervention, radiation exposure to the patient (radiation effective dose, mSv), and acute renal outcome with the change of creatinine, and major adverse cardiac events (MACE), such as cardiac death, target-vessel revascularization, and myocardial infarction during follow-up.
|
|
|
Results:
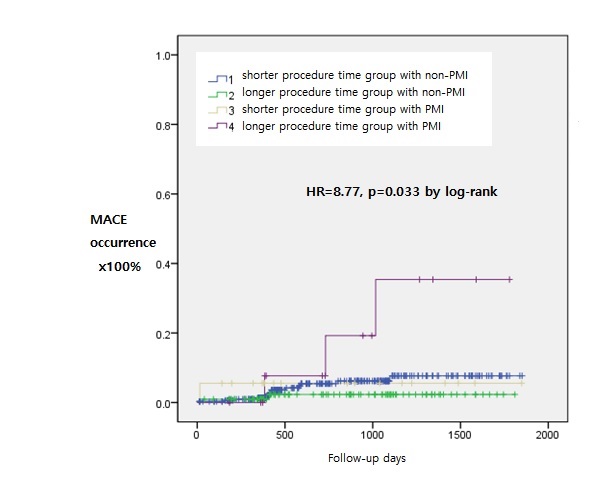
Significant independent risk factors for longer procedure-time were three kinds of wiring attempt (antegrade-only(ref) vs. retrograde-only, vs. hybrid-approach, odds ratio(OR)=5.40(95%confidence interval(CI)=1.65-17.60, p=0.005), OR=16.48, 95%CI=7.89-34.41, p<0.001), and the number of implanted stents (OR=1.82, 95%CI=1.24-2.67, p=0.002). Longer procedure-time group was likely to occur PMI (13.2% vs. 5.2%, p=0.004), and to be exposed higher radiation effective dose (mSv, 59.8¡¾34.9 vs. 127.9¡¾57.7, p<0.001), but not different significantly for acute renal outcome. Longer procedure-time with PMI group had significantly higher MACE rate than other groups, such as shorter procedure-time group or non-PMI group or longer procedure-time with non-PMI group (hazard ratio=8.77, p=0.033 by log-rank test).
 |
|
|
Conclusion:
Independent risk factors for longer procedure-time during CTO intervention were the kinds of wiring attempt, and the number of implanted stents. Longer procedure-time with PMI were strongly related to MACE occurrence after CTO intervention.
|
|