Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
ABS20190928_0004
| Stents (bare-metal, drug-eluting) | |
| Prognosis Risk Factors of Drug-Eluting Stent In-Stent Restenosis (DES-ISR) in Short-Term Outcomes | |
| Jianfeng Zheng1, hong qiu1 | |
| Fuwai Hospital, China1 | |
|
Background:
The mechanism and course of drug-eluting stent in-stent restenosis (DES-ISR) have not been fully clarified. Treatment of those patients remains a major challenge. The aim of this study was to determine the predictors for DES-ISR outcomes in short-term.
|
|
|
Methods:
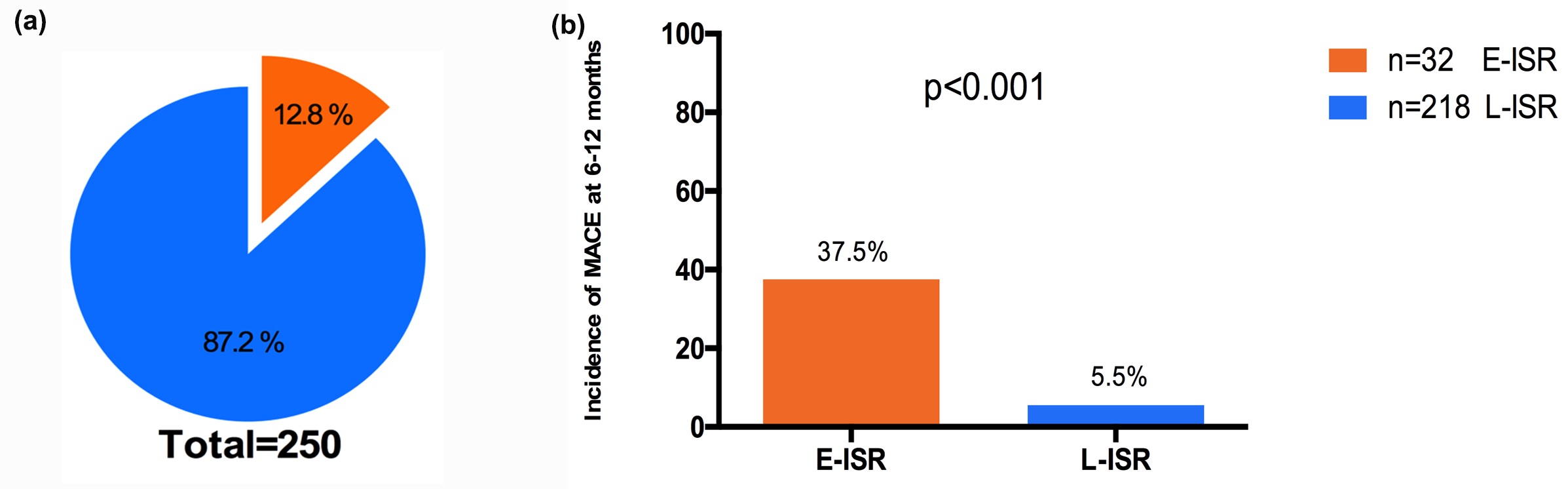
A total of 250 patients those had initial stent implantation in our hospital and readmitted to receive treatment for the reason of recurrent significant DES-ISR in 2016 were involved. Patients were categorized as early ISR (<12 months; E-ISR; n=32) and late ISR (¡Ã12 months; L-ISR; n=218). Associations between patient characteristics and clinical performance, as well as clinical outcomes after percutaneous coronary intervention (PCI) were evaluated. Primary composite endpoint of Major adverse cardiac events (MACE) included cardiac death, non-fatal myocardial infarction, or target lesion revascularization (TLR).
|
|
|
Results:
Most baseline characteristics were similar in both groups, except the period of ISR, initial pre-procedure TIMI, and some serum biochemical indicators. The incidence of MACE (37.5% vs 5.5%; p<0.001) and TLR (37.5% vs 5.0%; p<0.001) was higher in the E-ISR group. After multivariate analysis, E-ISR (odds ratio[OR], 13.267; [95% CI 4.984-35.311]; p<0.001) and left ventricular systolic dysfunction (odds ratio[OR], 6.317; [95% CI 1.145-34.843]; p=0.034) were the independent predictors for MACE among DES-ISR patients in short-term follow up of 6-12 months.
 |
|
|
Conclusion:
Early ISR and left ventricular systolic dysfunction were associated with the short-term outcome of MACE in DES-ISR patients. The results may benefit the risk stratification and secondary prevention after DES implantation in clinical practice.
|
|