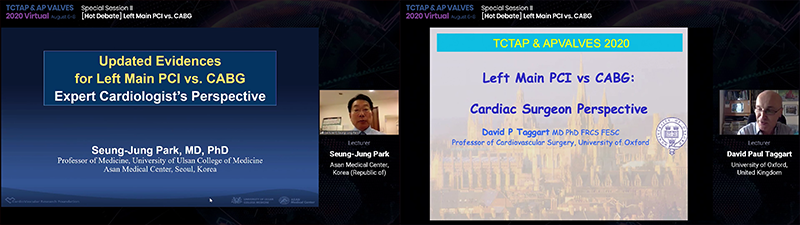
Cardiac Surgeon David Taggart, Interventional Cardiologist Seung-Jung Park Face Off in CABG Vs. PCI Debate
Park says ¡°LMCAD is no longer a surgical disease¡± while Taggart rebuts ¡°CABG a clear winner in left main¡±
Two prominent researchers went head to head in a dynamic TCTAP & AP VALVES VIRTUAL 2020 session over the optimal revascularization strategy for patients with left main coronary artery disease (LMCAD).

 The session, held online on Aug. 7, featured cardiac surgeon David Taggart from the University of Oxford and interventional cardiologist Seung-Jung Park from Asan Medical Center in Seoul, South Korea.
The session, held online on Aug. 7, featured cardiac surgeon David Taggart from the University of Oxford and interventional cardiologist Seung-Jung Park from Asan Medical Center in Seoul, South Korea.
The two professors delved into results of two large-sized trials - EXCEL and NOBLE - to compare outcomes of CABG and PCI with contemporary DES.
EXCEL and NOBLE are the two most well-known studies to examine PCI and CABG. However, these two trials produced conflicting results, raising further uncertainty regarding the best revascularization method for LMCAD.
Against this backdrop, Park explained the non-inferiority of PCI against CABG by pointing towards data stacked in favor of PCI - MAIN COMPARE, SYNTAX, PRECOMBAT - and saying that ¡°left main is no longer a surgical disease.¡±
Taggart then zoned in on the pitfalls of the landmark EXCEL study to dismiss the investigators¡¯ conclusion that PCI is non-inferior while emphasizing the superiority of CABG.
Although Taggart and Park took different sides of the debate, the two presenters along with six other internationally acclaimed cardiac surgeons and interventional cardiologists united under the front of the heart team approach.
Park stresses ¡°left main is no longer a surgical disease¡±
Park got the session rolling by pointing to the pooled data from 11 RCTs and 11,518 patients - ERACI II, ARTS, MASS-II, SoS, SYNTAX, PRECOMBAT, FREEDOM, VA CARDS, BEST, NOBLE, EXCEL - that was utilized for a patient-level meta-analysis that was published in the Lancet in 2016.
¡°Meta-analysis results at five years showed that bypass surgery had better outcomes than PCI,¡± Park said. ¡°But when looking at the impact of left main disease versus multi-vessel disease - there was no statistically significant difference between PCI and CABG in terms of all-cause mortality for left main disease. In multi-vessel disease, bypass surgery was better.¡±
Park explained that surgery was better for diabetic patients while no difference existed between PCI and CABG regarding non-diabetics in the meta-analysis.
¡°PCI and CABG were equivalent for left main disease but CABG was better for multi-vessel disease and diabetes at five years,¡± he added.
With the totality of evidence, Park noted that ¡°in the past 20 years, there were tremendous changes in the treatment patterns for left main disease, in that the real-world practice has already changed to include more than 60 percent of left main disease patients treated by PCI with drug eluting stents in recent years.¡±
But Park noted that EXCEL and NOBLE brought on ¡°clearly contradictory results¡± that required long-term comparative outcomes of PCI and CABG.
This long-term data came in the form of MAIN COMPARE 10-year, SYNYTAX 10-year, EXCEL 5-year, NOBLE 5-year, and the recently published PRECOMBAT 10-year.
MAIN-COMPARE results showed ¡°some cross-over where surgery was better¡± in that ¡°the outcomes were almost exactly the same until five years, whereas PCI was associated with higher risk of death and serious composite outcomes after five years and up to 10 years.¡±
SYNTAX 10-year results, meanwhile, showed ¡°no significant difference on mortality, Park said.
Finally, Park gave his take on EXCEL and NOBLE.
The EXCEL three-year results published in 2016 focused on the primary endpoints of all-cause death, stroke, or MI and showed ¡°absolutely no difference¡± between PCI and CABG, he said.
According to Park, EXCEL five-year results showed ¡°statistically no significant difference¡± but indicated ¡°a cross-over with incidence curves, with later trends favoring surgery. Regarding piecewise hazards of all-cause death, stroke, or MI, there were three distinct periods of varying relative risk favoring PCI early on and bypass surgery later on. All-cause death was also incrementally higher in PCI with 13 percent versus 9.9 percent in CABG, which was mainly driven by the difference in non-cardiovascular deaths (6.6 percent vs. 4.6 percent).¡±
¡°In conclusion, EXCEL five-year results showed that PCI with CoCr-EES and CABG in LMCAD with visually assessed low-to-intermediate SYNTAX scores resulted in similar rates of the clinically meaningful composite outcome of death, stroke, or MI at five years,¡± Park said.
¡°The early benefits of PCI due to reduced peri-procedural risk were attenuated by the greater number of events occurring during follow-up with CABG, such that at five years, the cumulative mean time free from adverse events was similar with both treatments,¡± he added.
Regarding NOBLE 5-years, Park noted that in LMCAD revascularization, ¡°PCI was associated with inferior clinical outcomes at five years compared to CABG. However, mortality was similar after the two procedures, although patients treated with PCI had higher rates of non-procedural myocardial infarction and repeat revascularization.¡±
¡°The most recent PRECOMBAT 10-year study also failed to demonstrate significant difference on mortality as well as composite events between PCI and CABG, while CABG was better in the subgroups of 3-vessel disease.¡±
Park summarized by saying, ¡°The updated evidence for left main PCI vs. CABG based on five to 10-year follow-up data shows that PCI with DES had similar clinical outcomes to CABG in terms of all-cause death and/or stroke for LMCAD.¡±
¡°PCI had higher rates of non-procedural MI and repeat revascularization compared to CABG, which may be related to incompletely treated combined triple-vessel disease,¡± he said. ¡°So we¡¯ve learned from all the data that complete revascularization with PCI had comparable clinical outcomes with CABG and that complete revascularization is an important practical issue for better outcomes regarding PCI.¡±
¡°From an expert cardiologist¡¯s perspective in 2020, PCI is a good alternative to CABG in isolated left main as well as left main with one- or two-vessel disease,¡± Park said. ¡°Even in left main with triple-vessel - in other words higher SYNTAX score - PCI is a good alternative to CABG when we incorporate the concept of complete revascularization, preferably with FFR. In other words, left main is no longer just a surgical disease.¡±
¡°CABG is a clear winner for left main¡±
Taggart fiercely rebutted Park¡¯s claims by zoning in on the EXCEL trial and saying that ¡°for multi-vessel disease without left main, CABG is a clear winner for all patients - at any level of SYNTAX score - and especially for diabetes.¡±
Taggart pointed to four major concerns of EXCEL.
The first - and major - concern related to the issue of the investigators ¡°changing¡± the three-year non-inferior statistical analysis to superiority at five-years, a move that the surgeon referred to as ¡°statistical trickery.¡±
In addition, EXCEL¡¯s ¡°faulty¡± interpretation of mortality data, a persistent failure to publish protocol specified MI data, and a failure of EXCEL investigators to share trial data were also major issues.
This is what blew up the controversy last year - in which Taggart found himself at the center at with EXCEL principal investigator Stone - and the subsequent fallout in which three major cardiothoracic surgery societies across the Atlantic - the European Association for Cardio-Thoracic Surgery (EACTS), American Association for Thoracic Surgery (AATS), and Society of Thoracic Surgeons (STS) - demanded independent re-analysis of the EXCEL results.
Taggart himself was the chairman of the surgical committee of EXCEL during the design and recruitment of the trial.
He noted that EXCEL is the largest and most definitive trial of PCI vs. CABG in left main disease and that ¡°the investigators, participants, and patients deserve enormous credit for participating in this trial.¡±
The University of Oxford was also the second largest recruiter of EXCEL patients worldwide having recruited 100 patients, a point Taggart stressed was a testament to the Oxford cardiologists and surgeons in determining the trial¡¯s success. Although Taggart said he wanted EXCEL to succeed and applauded their efforts, he noted that he could not ¡°turn a blind eye¡± to the true facts of what truly happened in the trial.
¡°For the record, there was no attempt in the EXCEL trial to manipulate or distort the data that was actually presented,¡± Taggart said. ¡°But there was a failure to present protocol-specified data that was vitally important to the true interpretation of the EXCEL trial.¡±
It was for this and a number of other reasons that Taggart finally withdrew authorship from the final manuscript- he couldn¡¯t agree with the interpretation of the data, he said.
The renowned surgeon highlighted four key rules for interpreting PCI and CABG data: determining whether the trial patients are reflective of real clinical practice, whether the duration of follow-up is a minimum of five or 10 years (such as PRECOMBAT), whether the study uses guideline-directed medical therapy (GDMT), and whether the data is examined before the published ¡°text manuscript.¡±
Taggart stressed that EXCEL fell short in adhering to these four key rules.
In particular, the primary outcome at three-years was ¡°non-inferiority¡± with an upper margin of 4.2 percent. At five-years however, Taggart said, ¡°without any discussion or explanation,¡± the primary outcome was changed to superiority.
¡°We should have, in fact, rejected the theory that PCI is equivalent to CABG at five years as the 95% CI extended up to 6.5 percent and therefore crossed the noninferiority margin, and - it really begs the question - where were the statisticians and was the NEJM asleep?¡± Taggart asked tongue-in-cheek.
The second issue was mortality at five years. Taggart pointed out that ¡°keeping in mind that these were relatively young patients with a median age of 66 years and low to intermediate severity disease, there was a 38 percent increase in the risk of death at five years. And if you look at the survival, you can see that they are rapidly accelerating in divergence. There was no difference in stroke; there was also a significant difference in ischemia driven revascularization in favor of CABG.¡±
However, in the NEJM paper, Stone and investigators had concluded that ¡°in patients with left main coronary artery disease of low or intermediate anatomical complexity, there was no significant difference between PCI and CABG with respect to the rate of the composite outcome of death, stroke, or myocardial infarction at five years.¡±
¡°While [the NEJM conclusion] may be technically true,¡± Taggart said, ¡°I don¡¯t think it was really a fair presentation of what really happened in the EXCEL trial.¡±
Pointing to the data, Taggart explained that there was no difference between PCI and CABG regarding the primary and secondary outcome from 0 to 30 days. However, CABG was ¡°penalized¡± for having a much higher procedural incidence of MI using a new, previously undefined biochemical definition.
Even though there was no difference in death, stroke, MI at 30 days to one year with higher revascularization in PCI, and PCI had a larger increase in death, MI, revascularization from one to five years, Taggart criticized that all of this was still interpreted as no difference between PCI and CABG.
In addition to the ¡°unfair¡± presentation of EXCEL, Taggart also pointed out that EXCEL protocol repeatedly specified that it would not only report a new biochemical definition of procedural MI (SCAI) - but also publish the universal definition of MI (UDMI). This protocol was the ¡°vital safety check¡± to compare the two definitions both in the EXCEL and compare with other studies.
¡°But despite assurances that the UDMI would be published, only the new definition was used and that drove the composite endpoint, which was far higher in the CABG arm,¡± Taggart said. ¡°Interestingly, the UDMI data was leaked to BBC, and they reported that the data showed a far higher rate of MI in the PCI group.¡±
To capitalize on his point, Taggart relied on an independent analysis by New York Presbyterian - Weill Cornell Medical Center¡¯s cardiac surgeon Mario F.L. Gaudino who analyzed what the data would look like if EXCEL excluded peri-procedural MIs.
¡°If you exclude peri-procedural MI based on the analysis by Gaudino, then CABG is a clear winner, not only for the composite endpoint, but also for the individual components of death and non-procedural MI - or in other words real MI,¡± Taggart explained. ¡°This also applies for the overall incidence of repeat revascularizations.¡±
The final EXCEL concern was the fact that the investigators were not prepared to share the data, Taggart said.
¡°This begs the question - why would that be? It is conventional practice to share data if there is a legitimate request,¡± the surgeon said. ¡°It is also puzzling since several of the EXCEL authors published numerous meta-analyses with data from other studies.¡±
EXCEL had, in conclusion, ignited more debate than solved any problems, Taggart noted, and he criticized that you can pick and choose from any existing data to either support or refute the EXCEL findings.
¡°A study published in the EHJ this year by interventional cardiologists takes the largest and most definitive trial of EXCEL and waters it down with older, smaller, weaker studies until any mortality benefit of CABG disappears,¡± Taggart pointed out.
¡°Meanwhile, if you look at a Bayesian interpretation of the EXCEL trial published in JAMA Internal Medicine about a month ago by a non-interventional cardiologist, he specifically suggested - whether based on EXCEL results alone or on the totality of available evidence - that PCI was associated with inferior long-term results for all events, including mortality, compared with CABG for LMCAD.¡±
Taggart also brought up NOBLE and compared it with EXCEL, outlining stark differences.
¡°Even though the mean age in NOBLE and EXCEL were the same at 66 years, the mean SYNTAX score was lower in NOBLE with 22 versus 26 in EXCEL,¡± Taggart said. ¡°NOBLE also had less diabetes - 15 percent versus 30 percent in EXCEL.¡±
¡°So the NOBLE five-year follow up showed that the trial is conclusive: PCI remained inferior to CABG in five year MACCE, and CABG was superior to PCI,¡± he said.
¡°This also applies to the group with a SYNTAX score less than 23, and all-cause mortality was similar for PCI and CABG - not to mention PCI resulted in higher rates of non-procedural MI and repeat revascularization,¡± he added.
Wrapping up the debate and acknowledging his debate counterpart Park, Taggart highlighted the superiority of CABG.
¡°To summarize and conclude, my take is that for patients with multi-vessel disease and no left main, CABG is a clear winner for all,¡± he said. ¡°Especially for left main disease, CABG is a clear winner for those with more severe disease with SYNTAX scores greater than 32.¡±
¡±The two largest trials of LMCAD in patients with low-to-intermediate disease severity showed that CABG is superior for mortality [in EXCEL], non-procedural MI, and repeat revascularization [in both EXCEL and NOBLE].¡±
Heart team approach agreed upon by all
Following the dynamic debate, the six moderators and panelists chimed in on the heated CABG, PCI issue with all eight physicians allied under the objective of finding the best heart treatment for their patients.
Interventional cardiologist Antonio Colombo kicked off the discussion by highlighting the importance of the individual patient.
¡°Both views had a lot of similarities¡± Colombo said. ¡°I tend to agree with a lot of Taggart¡¯s views but we need to look at subgroups - I don¡¯t like clumping multi-vessel altogether and clumping left main altogether.¡±
¡°In general, CABG is an appropriate choice for a young multi-vessel patient in the hands of a good surgical team,¡± Colombo continued. ¡°On the other hand, PCI may be better in elderly patients with some more discrete multi-vessel disease.¡±
¡°We need to extract general messages from these trials and then become practitioners by applying the data to the patient in front of us,¡± Colombo stated.
¡°Let us not be dogmatic - we have the SYNTAX score, we have the age, we have the extent of the disease, among others. I like to be more punctual and specific to the patient in front of us,¡± Colombo stressed.
Based on Colombo¡¯s comment, debate moderator and interventional cardiologist Spencer B. King III, asked panelists how surgeons and interventional cardiologists alike can discern the correct patients for either PCI or CABG.
¡°As usual Antonio is providing a lot of wisdom,¡± King said. ¡°So I would like to ask - among sub-patients - how we can define the patients who should not be for PCI.¡±
In response to King¡¯s question, interventional cardiologist Alan C. Yeung noted that communication between surgeons and interventional cardiologists is crucial. ¡°You don¡¯t always necessarily have to get a group of interventional cardiologists and a group of cardiac surgeons together to decide on one patient,¡± Yeung said.
¡°But certainly, I think any patient with left main disease should have a surgical consult at least for a balanced view because, as you know, it is easy for us to be in the cath lab to try and fix the problem,¡± Yeung continued, ¡°but it¡¯s always wise to step back and have a second opinion.¡±
¡°We tend to lump everything together because we want the power to show something,¡± Yeung said. ¡°But when you lump everything together, you miss the details of the patient and end up with one conclusion for all - and that¡¯s impossible for left main disease, which is very heterogeneous.¡±
¡°It¡¯s important to un-lump the patient - meaning when you see the patient, you need to look at all the factors. There are patients we shouldn¡¯t do such as left main with lots of calcification around the bifurcation and proximal LAD or LCX - technically, we could do everyone but the most important question is, should we do it. And that¡¯s when we should work with our surgical colleagues to give a balanced view,¡± he said.
Upon Yeung¡¯s comment, Colombo chimed in by saying, ¡°If I have in front of me a 55-year-old gentleman with a distal left main lesion that can be treated with one single 4-mm stent and focal lesion that can be treated with one short stent and another lesion in the big OM that can treated with another short stent - I am not making a mistake in offering PCI. However, I¡¯m also not making a mistake in offering CABG. If I offer PCI to this patient, I have to tell him that the risk of revascularization is higher than bypass and the risk of death and MI is probably similar. But this is a very specific subset patient.¡±
Cardiac surgeon Mario F.L. Gaudino from Weill Cornell Medicine in New York largely kept silent until moderator Domenico Pagano from University Hospital Birmingham-Queen Elizabeth directed a question towards him. However, when Gaudino spoke, he hit major points that had all panelists nodding and concluded with, not a statement, but a rather important question.
¡°It¡¯s reassuring for someone like me that both interventional cardiologists and surgeons agree that we should individualize the treatment to the patient,¡± Gaudino began. ¡°And there is no clear-cut boundary or golden rule - not everyone should get CABG and not everyone should get PCI. It¡¯s an individualized decision, and I share Professor Colombo¡¯s approach.¡±
¡°Trials give you the information of the average patient - but the reality is the average patient does not exist,¡± Gaudino said. ¡°We have different patients that are very often at different ends of the spectrum and we have to tailor our decision to the individual patient characteristic.¡±
¡°There is no doubt in my mind that PCI has a smoother post-operative course, but the long-term outcome is better with CABG,¡± he continued. ¡°So depending where your patient fits on the spectrum, you must make a decision with your colleague in the heart team.¡±
Then Gaudino launched into the pivotal question.
¡°The big concern I have is - after the EXCEL controversy - the vital heart team progress made following the SYNTAX trial has been jeopardized,¡± Gaudino said. ¡°EXCEL was a major dividing factor within the cardiology community.¡±
¡°The European Association of Cardiothoracic Surgery (EACTS) withdrew from the guideline - and even though I don¡¯t think it should guide our practice -not having a guideline in left main at the moment is disorienting,¡± he said.
Gaudino then asked the speakers, moderators, and panelists whether the heart team approach can recover from the EXCEL fallout.
Pagano, who is also the EACTS Secretary General, responded by saying ¡°When BBC first made the program regarding the EXCEL allegations, the EACTS did not feel - for a number of scientific and professional issues raised - that those guidelines could be trusted anymore.¡±
¡°However, we believe strongly in the concept of the heart team,¡± Pagano said. ¡°This should not be used as an opportunity to break the heart team. It should be used as an opportunity for the heart team to become closer for the benefit of the patient.¡±
In a similar vein, interventional cardiologist Duk-Woo Park pointed out that the heart team approach in revascularization approach is - in fact - crucial. Equally crucial, however, is the heart team approach in interpreting trial data.
¡°We emphasize the heart team discussion in taking care of patients for revascularization,¡± Park said. ¡°This concept should also be applied to trial interpretations for an optimal interpretation and bias reduction.¡±
With all moderators, speakers, and panelists involved in the discussion, King wrapped up the session with a humorous anecdote and a question directed at Taggart that united all panelists.
¡°Many years ago, left main equaled surgery - that was easy,¡± King said. ¡°Now we go to the opposite end of the spectrum where we have complex patients and - I find - many times, a surgeon says ¡®this is left main, complex, high risk patient - alright send the patient to PCI.¡¯¡±
¡°We used to send very complex patients for surgery and surgeons would never turn them down, even if they were at very high risk of dying - but now the surgeon has a way out - they can say let¡¯s see interventional cardiologists take a shot with PCI,¡± King said.
Then King asked, ¡°So David [Taggart] - I would like to ask - do you turn anyone down?¡±
And without missing a beat Taggart replied, ¡°Absolutely, yes. At Oxford, we have a superb heart team so we haven¡¯t been impacted negatively but there are many places in the world where many heart patients don¡¯t get a heart team discussion.¡±
¡°Are there some patients who should be done by PCI? Clearly yes,¡± Taggart said. ¡°Not just frail, old, sick patients, but I think even younger patients with true ostial and mid-shaft left main without additional proximal coronary disease do well with stents.¡±
With all panelists smiling, Taggart closed the session saying, ¡°The real advantage of the heart team is that it individualizes the decision for the individual patient.¡±
Edited by
Pil Hyung Lee, MD
Seosan Jungang Hospital, Korea (Republic of)
Written by