Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-012
Using Distal Protection Device in Native Coronary Artery for Treatment of ACS With Heavy Burden of Thrombi
By Yen-Liang Lin, Mu-Yang Hsieh
Presenter
Yen-Liang Lin
Authors
Yen-Liang Lin1, Mu-Yang Hsieh2
Affiliation
National Taiwan University Hospital Hsinchu branch, Taiwan1, National Taiwan University Hospital, Taiwan2,
View Study Report
TCTAP C-012
CORONARY - Acute Coronary Syndromes (STEMI, NSTE-ACS)
Using Distal Protection Device in Native Coronary Artery for Treatment of ACS With Heavy Burden of Thrombi
Yen-Liang Lin1, Mu-Yang Hsieh2
National Taiwan University Hospital Hsinchu branch, Taiwan1, National Taiwan University Hospital, Taiwan2,
Clinical Information
Patient initials or Identifier Number
TJZ
Relevant Clinical History and Physical Exam
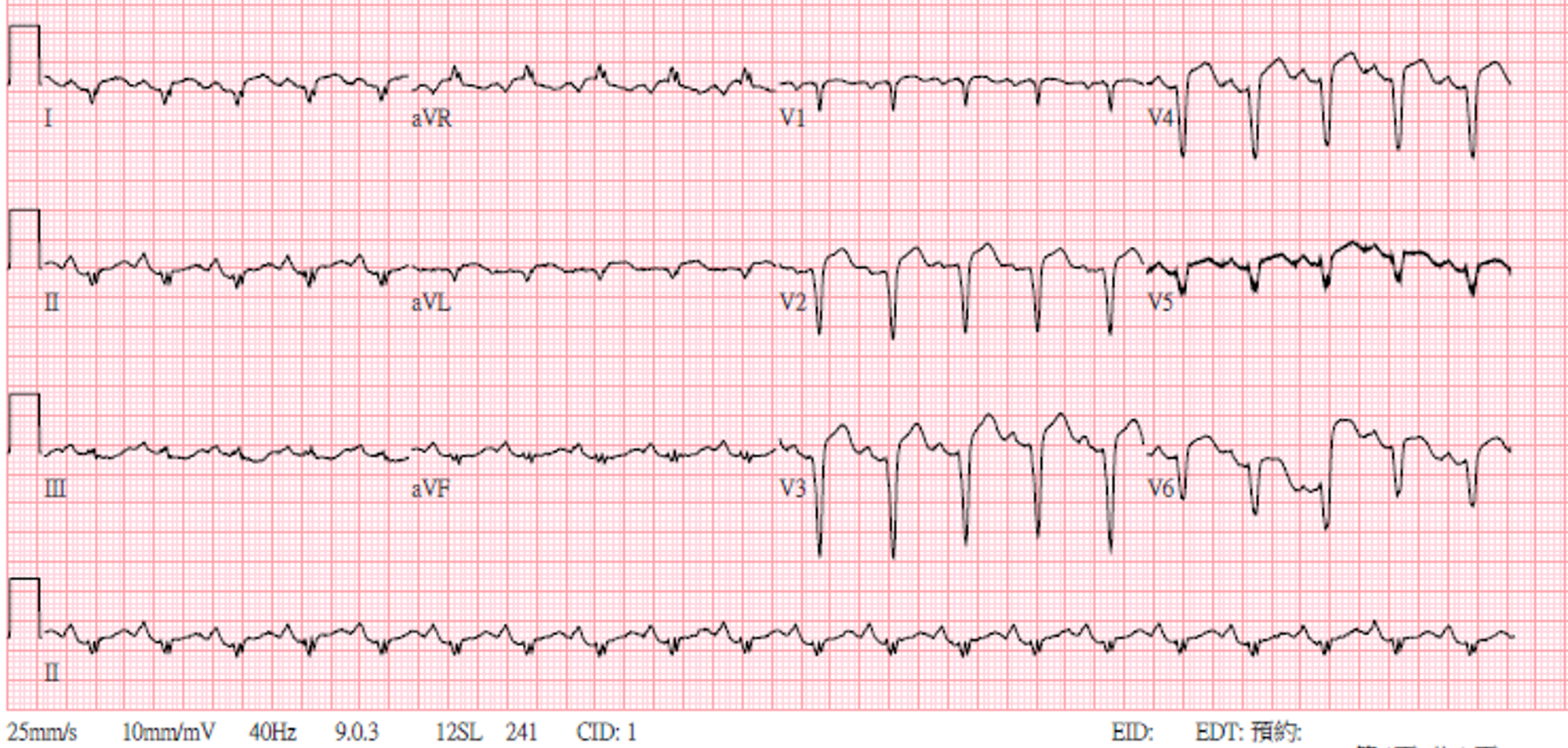
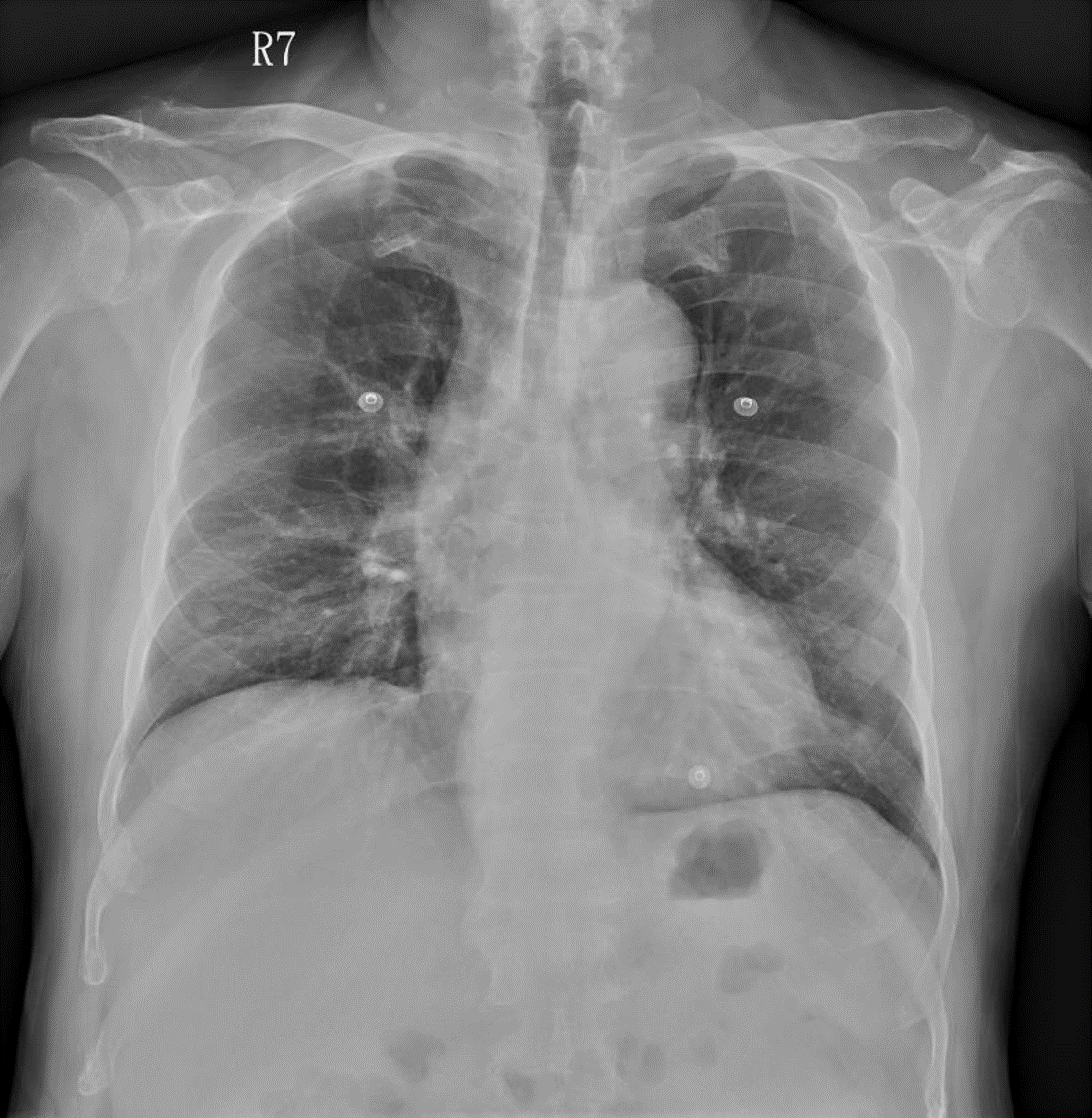
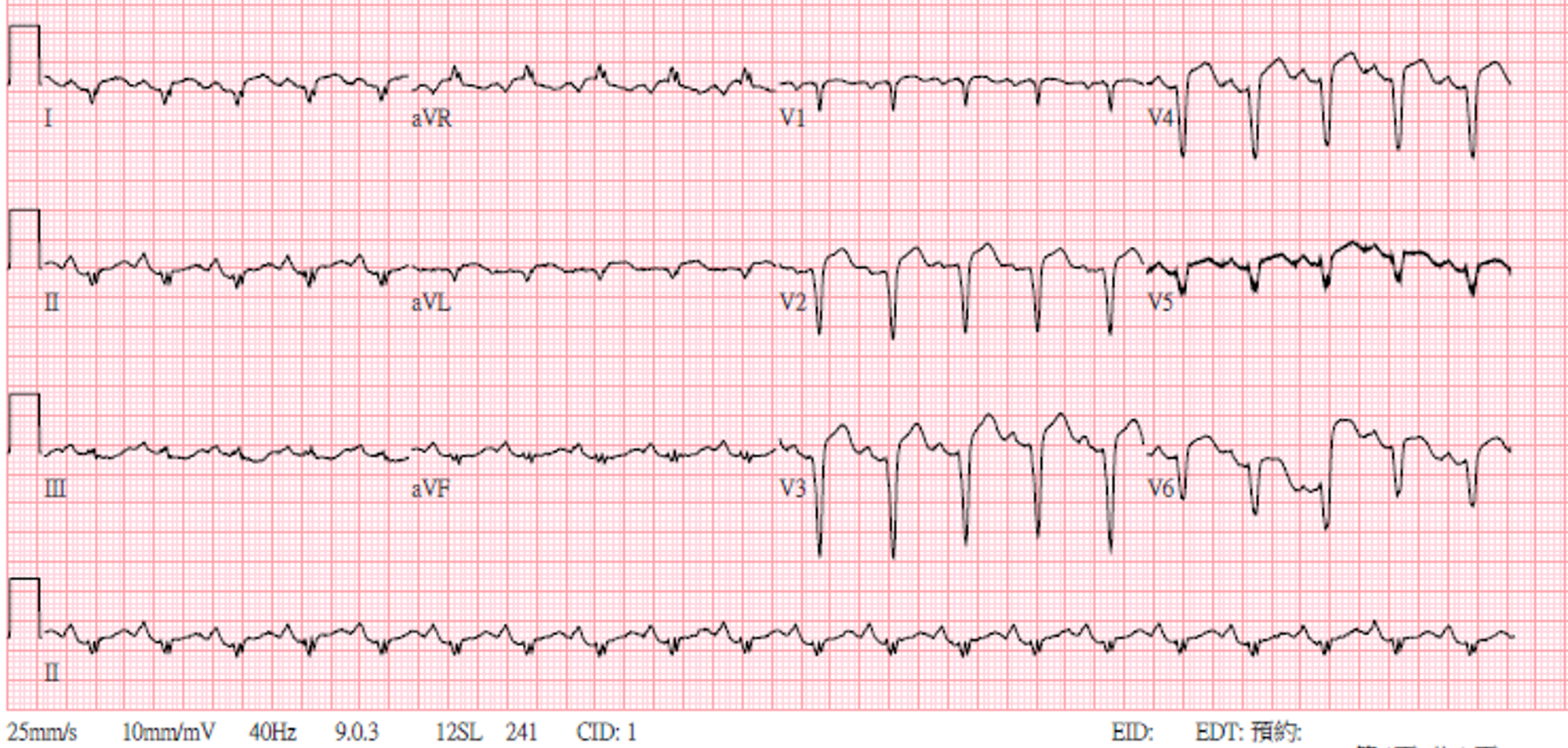
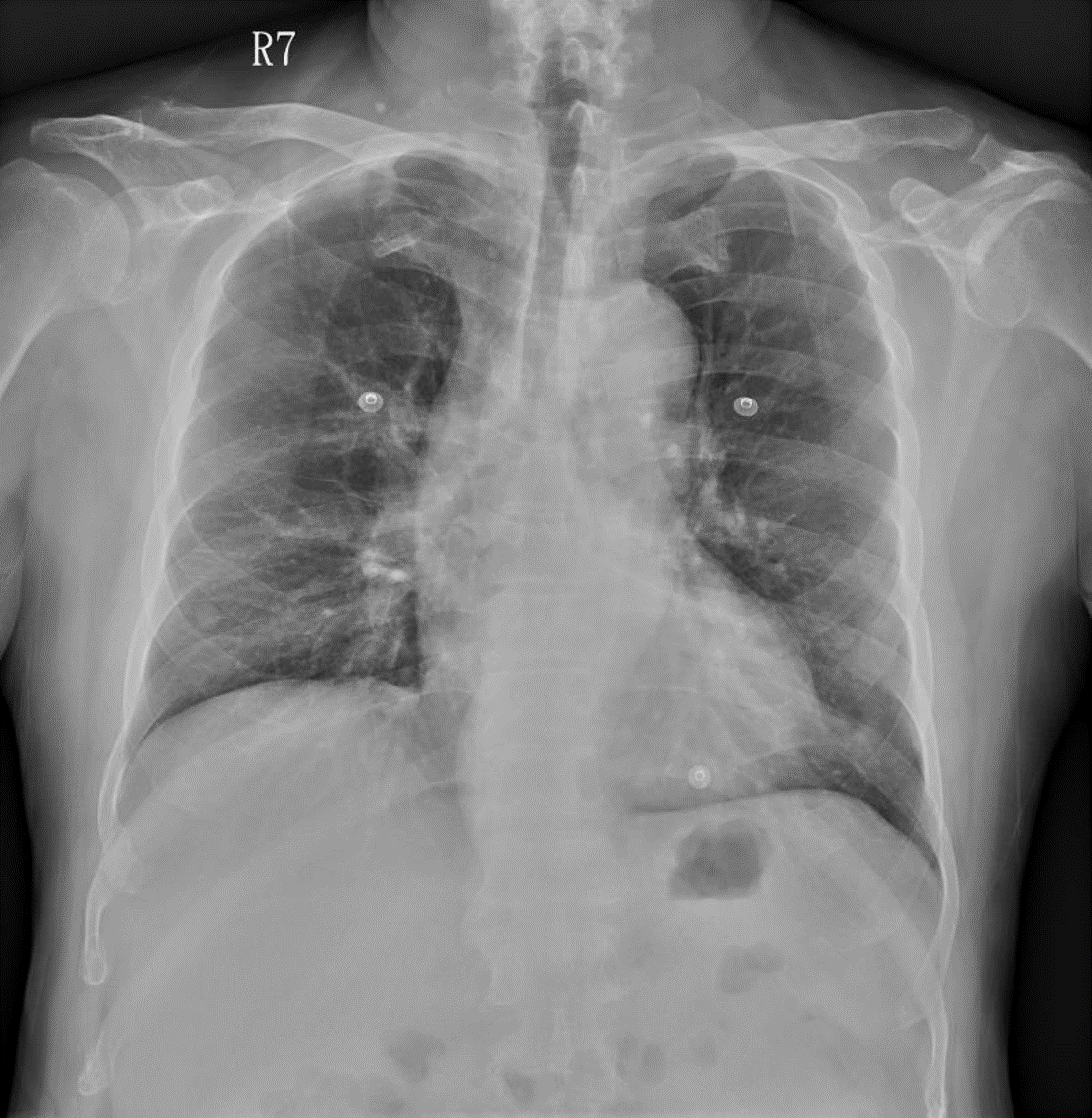
A 58-year-old man presented to ER with chest pain and diaphoresis for 1 day. He had poor controlled hypertension and habits of smoking for 30 years. The initial vital signs included HR 124 bpm and BP 149/103 mmHg. Physical exams showed regular heart beat without obvious heart murmur, clear breath sound, and no jugular vein engorgement. The ECG revealed sinus tachycardia with QS pattern and ST elevation over V1-V6 leads. Chest X-ray showed mild cardiomegaly without pleural effusion or lung edema.
Relevant Test Results Prior to Catheterization
Laboratory data disclosed leukocytosis (WBC 18.53 k/uL), normal renal function with hyponatremia (Cre 0.74 mg/dL, Na 129 mmol/L, K 3.5 mmol/L), impaired hapatic function (ALT 111 U/L), and elevated cardiac enzyme (troponin-T 5129 ng/L). Bedside echocardiogram revealed reduced left ventricular systolic function (ejection fraction 33.5%), with regional wall motion abnormality at septal and anterior wall. Dual antiplatelet with aspirin and prasugrel were prescribed prior to catheterization.
Relevant Catheterization Findings
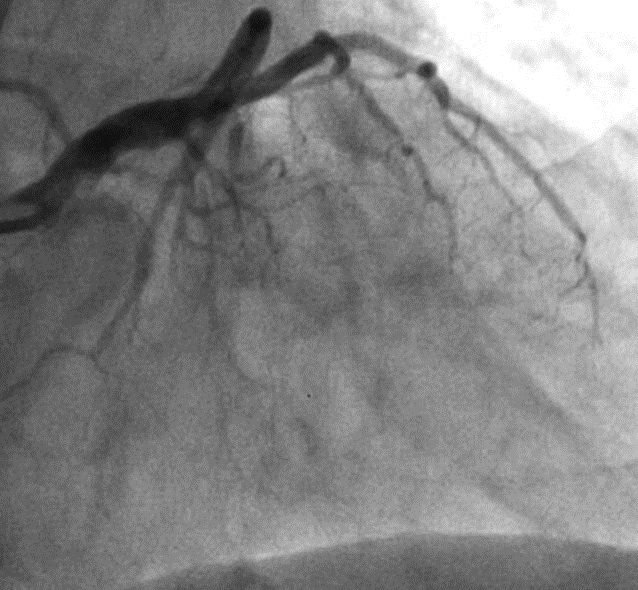
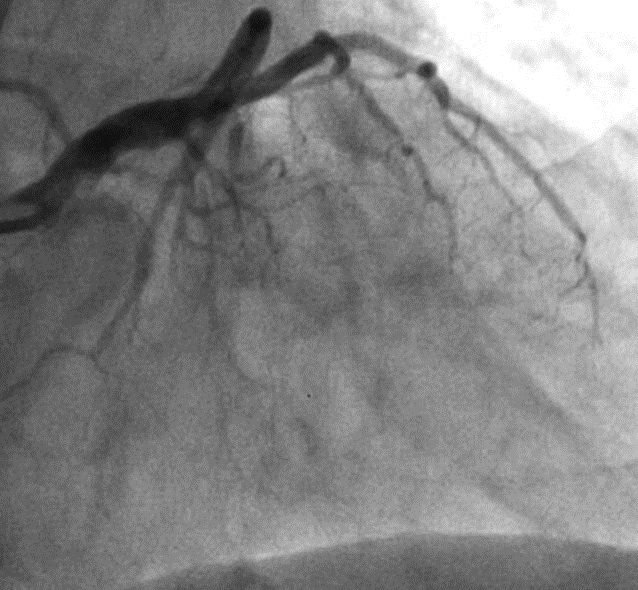
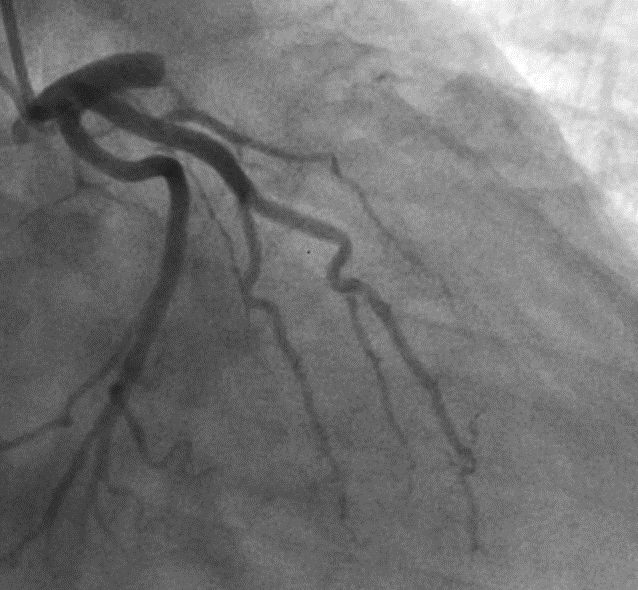
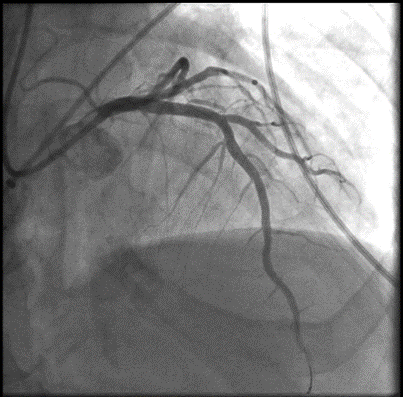
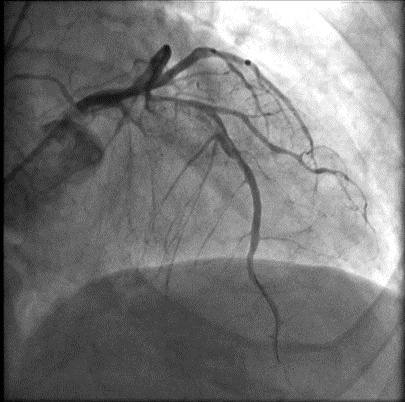
The diagnostic coronary angiogram revealed total occlusion from proximal left anterior descending artery (LAD), and there was no collateral from other coronary arteries. Calcification was also noticed at middle part of LAD.
Interventional Management
Procedural Step
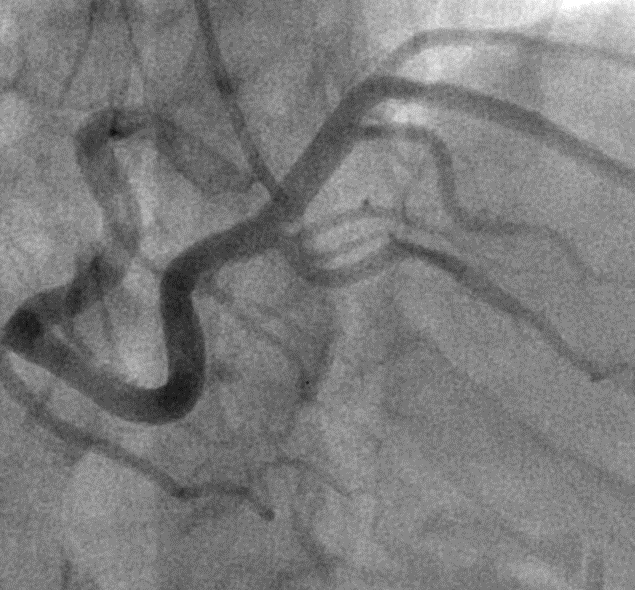
First PCI:1. Engaged guiding catheter 6Fr BL3.5 to left main artery, and gave tirofiban infusion2. Advanced a wire to left circumflex artery (LCX) for support, and another wire to left anterior descending artery (LAD) through hard thrombi3. Performed thrombosuction to LAD with 6Fr Thrombuster, and only achieved TIMI 1 flow4. Performed balloon angioplasty to LAD with balloon size 2.0*15 mm5. Ended up with TIMI 2 flow and much thrombi
Between two PCI:1. Tirofiban infusion followed by heparin infusion was given for thrombolysis.2. Intermittent angina with hypotension developed after first PCI.3. Intra-aortic balloon pump was placed for suspicious coronary hypoperfusion.
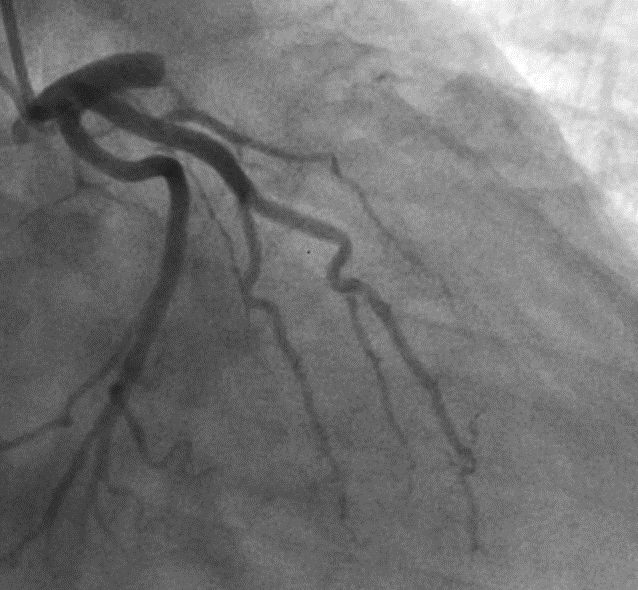
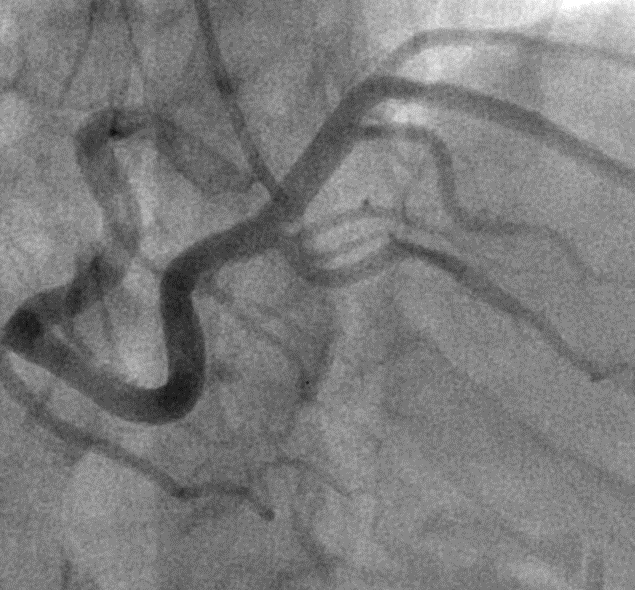
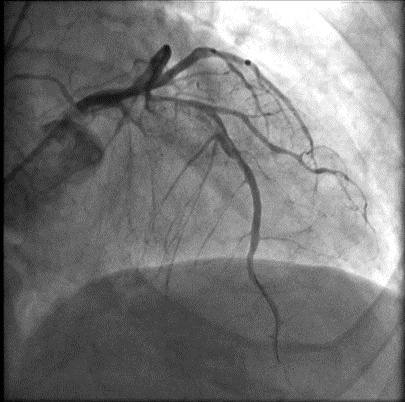
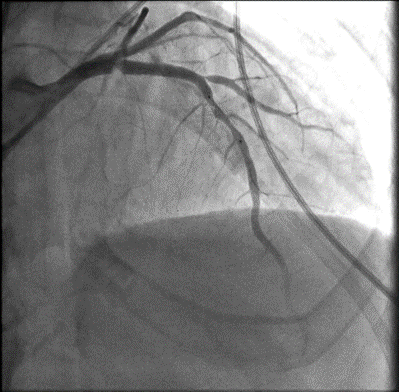
Second PCI (2 days later):1. Engaged guiding catheter 7Fr BL3.5 to left main artery, and noticed only TIMI 2 flow of LAD with much thrombi2. Advanced a wire to LAD, and placed a distal protection device "Spider Filter"3. Performed balloon angioplasty to LAD with balloon size 3.0*15 mm4. Deployed a bare metal stent "Rebel 4.0*32 mm" to LAD5. Performed post-dilatation by non-compliant balloon to stent edge with balloon size 4.5*15 mm6. Noticed thrombi in the Spider Filter and a huge thrombus at stent edge7. Gave urokinase infusion, but thrombi still existed8. Performed thrombosuction through guiding catheter 7Fr BL3.5, and the huge thrombus was retrieved9. Removed Spider Filter, and noticed thrombi inside device10. Performed post-dilatation by non-compliant balloon again11. Ended up with TIMI 3 flow and improved BP
Between two PCI:1. Tirofiban infusion followed by heparin infusion was given for thrombolysis.2. Intermittent angina with hypotension developed after first PCI.3. Intra-aortic balloon pump was placed for suspicious coronary hypoperfusion.
Second PCI (2 days later):1. Engaged guiding catheter 7Fr BL3.5 to left main artery, and noticed only TIMI 2 flow of LAD with much thrombi2. Advanced a wire to LAD, and placed a distal protection device "Spider Filter"3. Performed balloon angioplasty to LAD with balloon size 3.0*15 mm4. Deployed a bare metal stent "Rebel 4.0*32 mm" to LAD5. Performed post-dilatation by non-compliant balloon to stent edge with balloon size 4.5*15 mm6. Noticed thrombi in the Spider Filter and a huge thrombus at stent edge7. Gave urokinase infusion, but thrombi still existed8. Performed thrombosuction through guiding catheter 7Fr BL3.5, and the huge thrombus was retrieved9. Removed Spider Filter, and noticed thrombi inside device10. Performed post-dilatation by non-compliant balloon again11. Ended up with TIMI 3 flow and improved BP
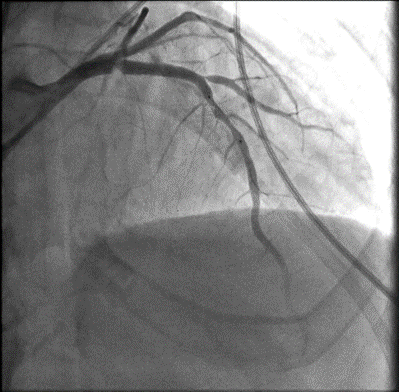
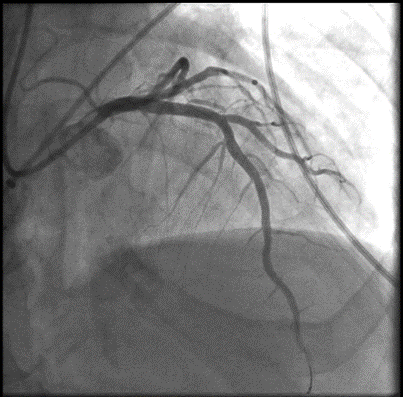
Case Summary
This is a STEMI case who presents more than 12 hours after symptom onset. Heavy burden of thrombi was observed from coronary angiogram. The efficacy of thrombolytic agent and aspiration catheter was limited during the first PCI. In order to prevent thrombus dislodgement, we placed a distal protection device before stent deployment. Manual aspiration directly through guiding catheter was also used for huge thrombus retrieval. There was absence of no reflow phenomenon during the procedure, and no major adverse cardiac events was noticed in the following 1 year. Distal protection device can be considered as a choice for preventing no reflow phenomenon in cases with heavy burden of thrombi.


