Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-191
Two Faces of Valve Atresia in Rural Area: A Case Series
By Tiara Larasati Jaya Putri, Markz Sinurat
Presenter
Tiara Larasati Jaya Putri
Authors
Tiara Larasati Jaya Putri1, Markz Sinurat2
Affiliation
RSUD Cileungsi, Indonesia1, Korea University Guro Hospital, Indonesia2,
View Study Report
TCTAP C-191
STRUCTURAL HEART DISEASE - Others (Structural Heart Disease)
Two Faces of Valve Atresia in Rural Area: A Case Series
Tiara Larasati Jaya Putri1, Markz Sinurat2
RSUD Cileungsi, Indonesia1, Korea University Guro Hospital, Indonesia2,
Clinical Information
Patient initials or Identifier Number
A & N
Relevant Clinical History and Physical Exam
In the first case, A 5 y.o boy was consulted due to recurrent shortness of breath. The patient has a history of uncorrected CHD. Physical examination showed lethargy, RR 32x/min, HR 89 bpm, Oxygen saturation 80% on room air and clubbing fingers. In the second case, A newborn girl was consulted due to desaturation and cyanosis. The APGAR score was 6/7. Physical examination showed central cyanosis with RR 60x/min, HR 166 bpm, and Oxygen saturation of 40% on room air.
Relevant Test Results Prior to Catheterization
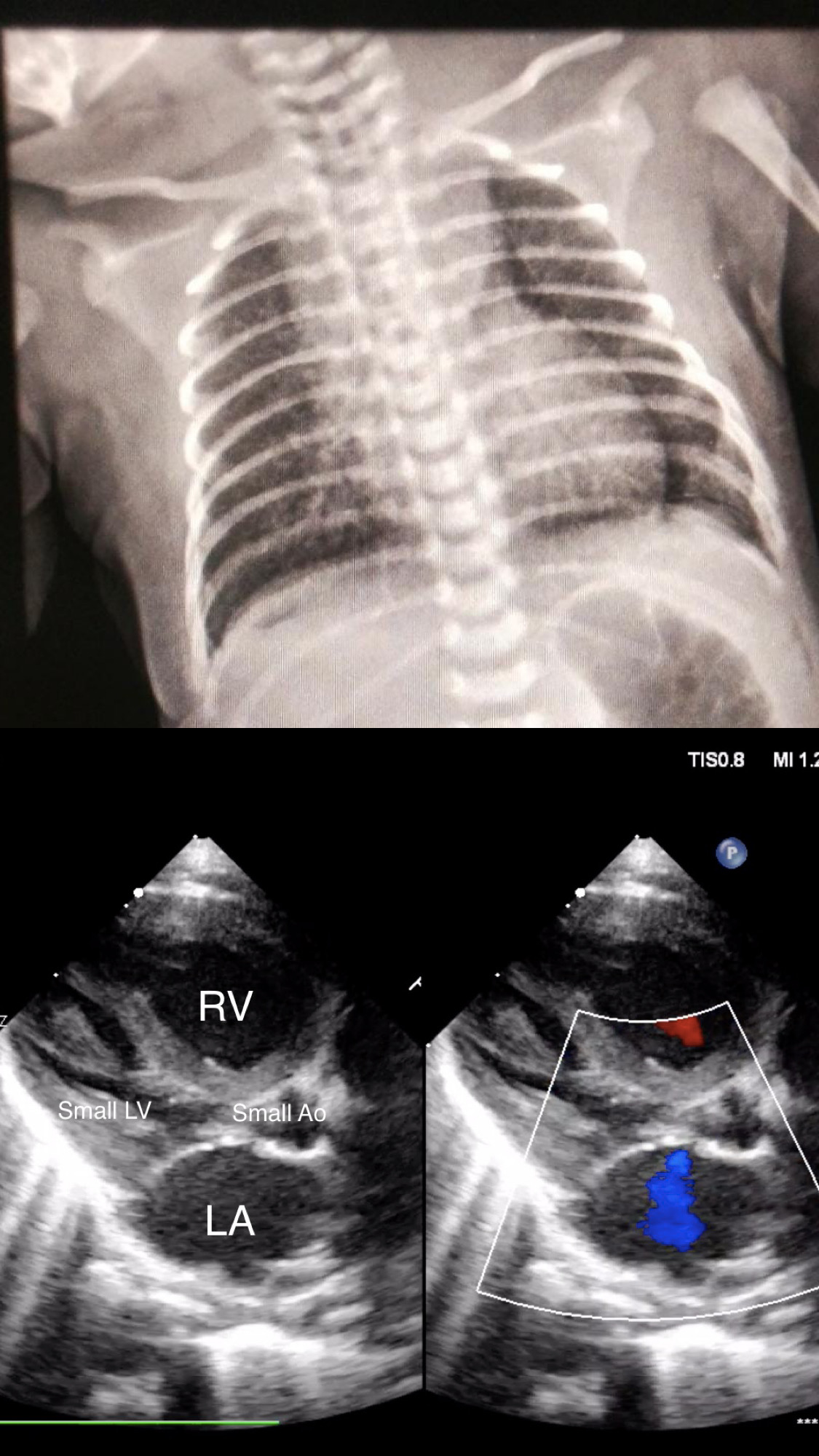
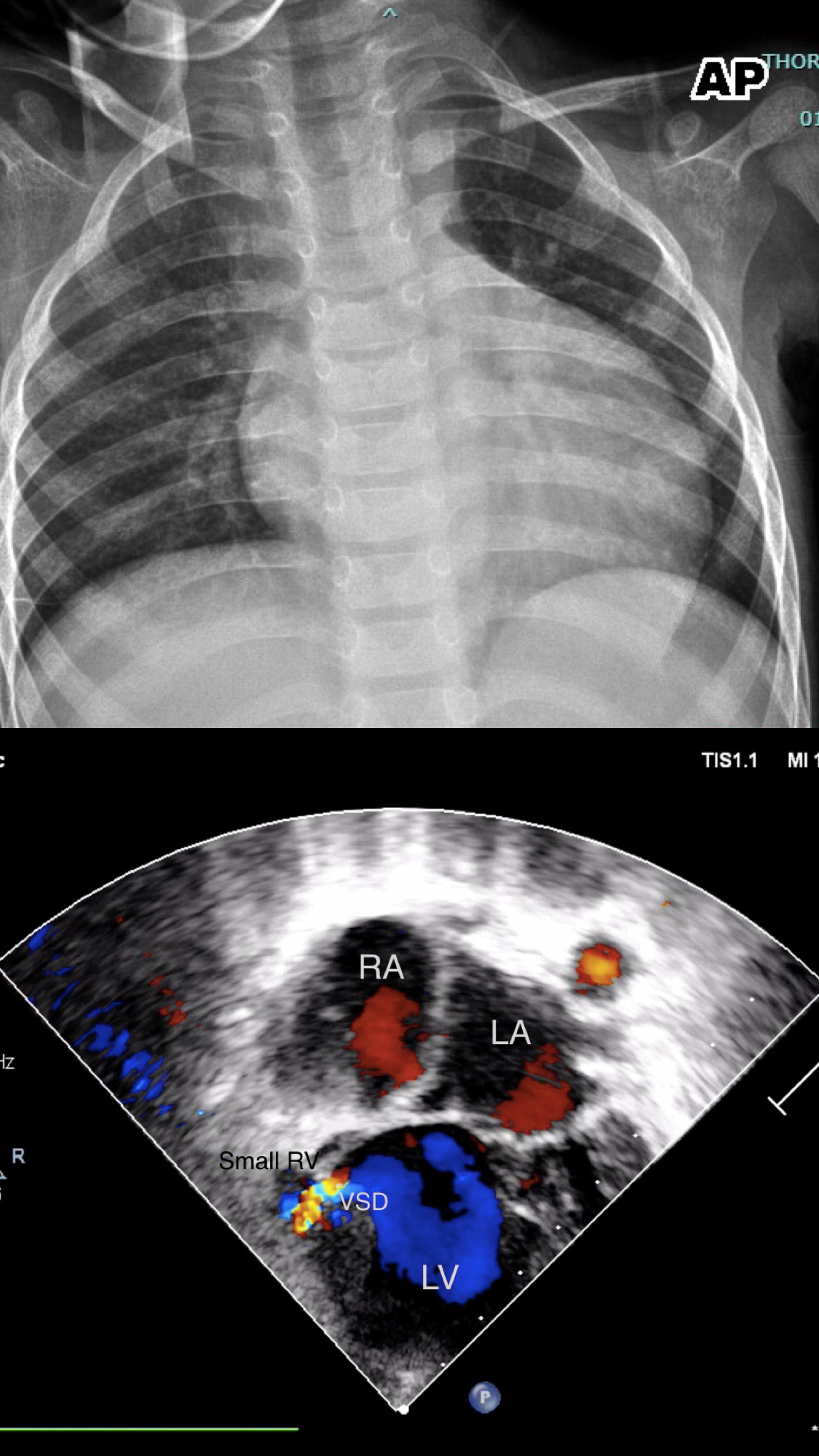
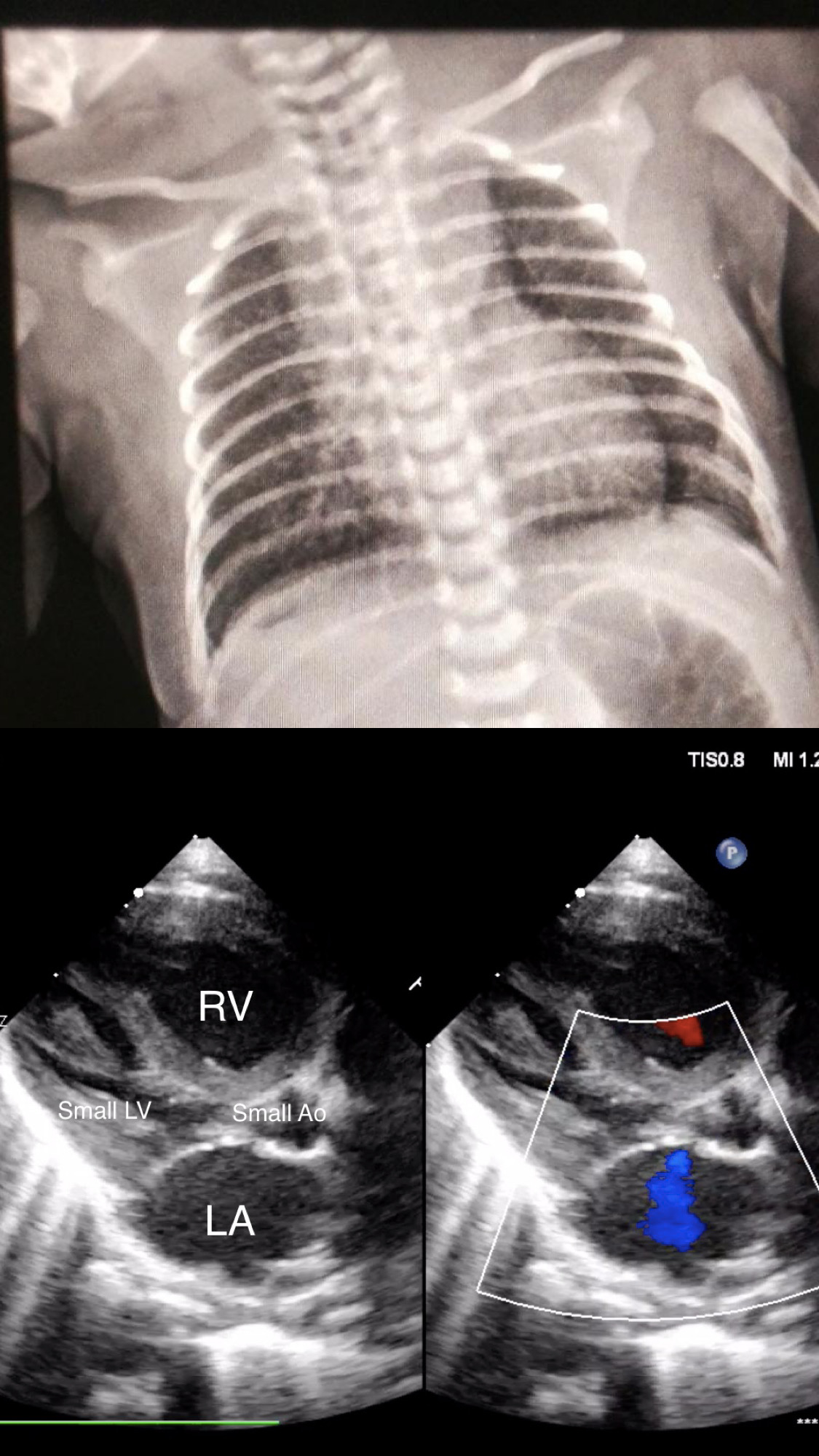
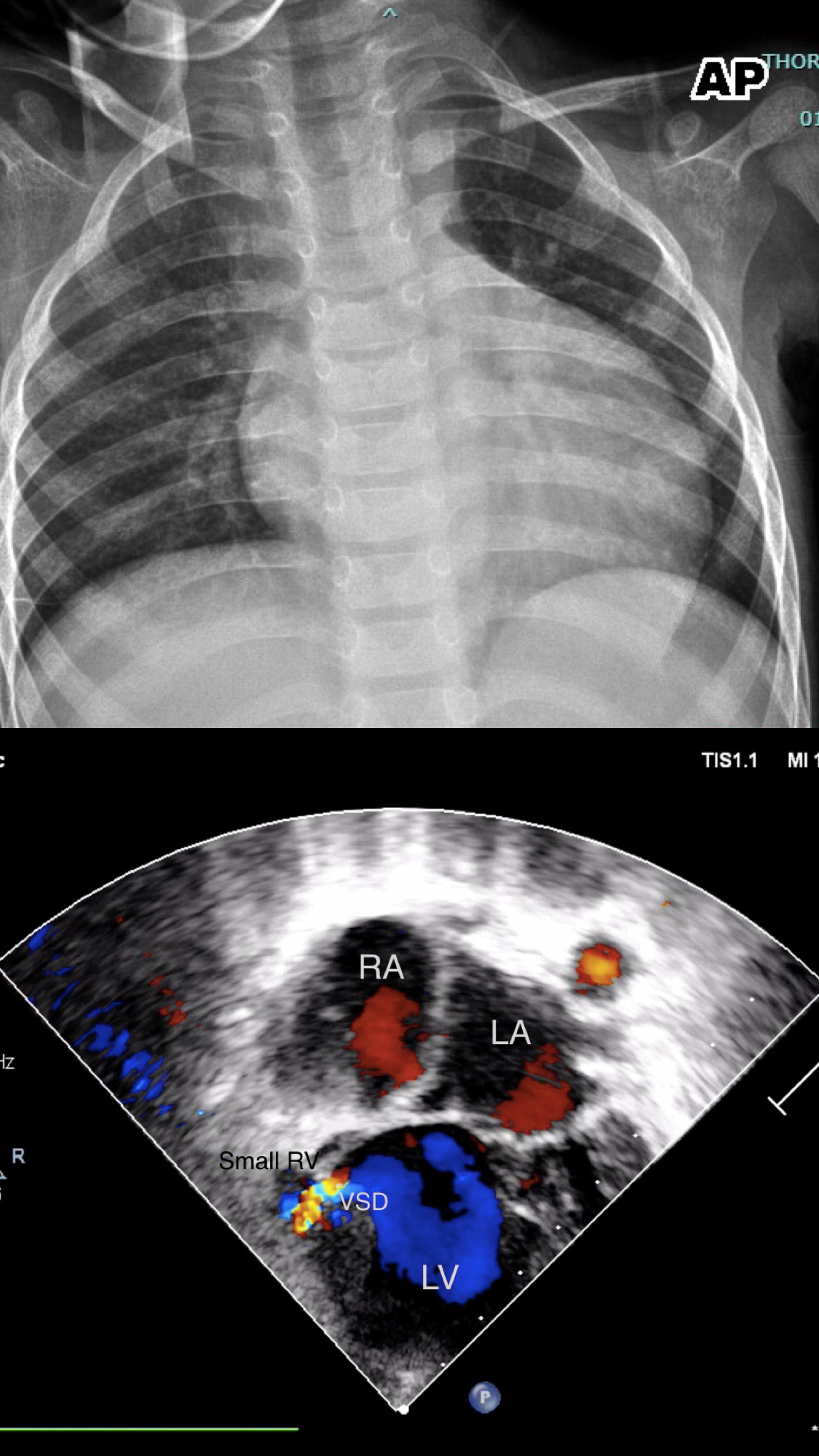
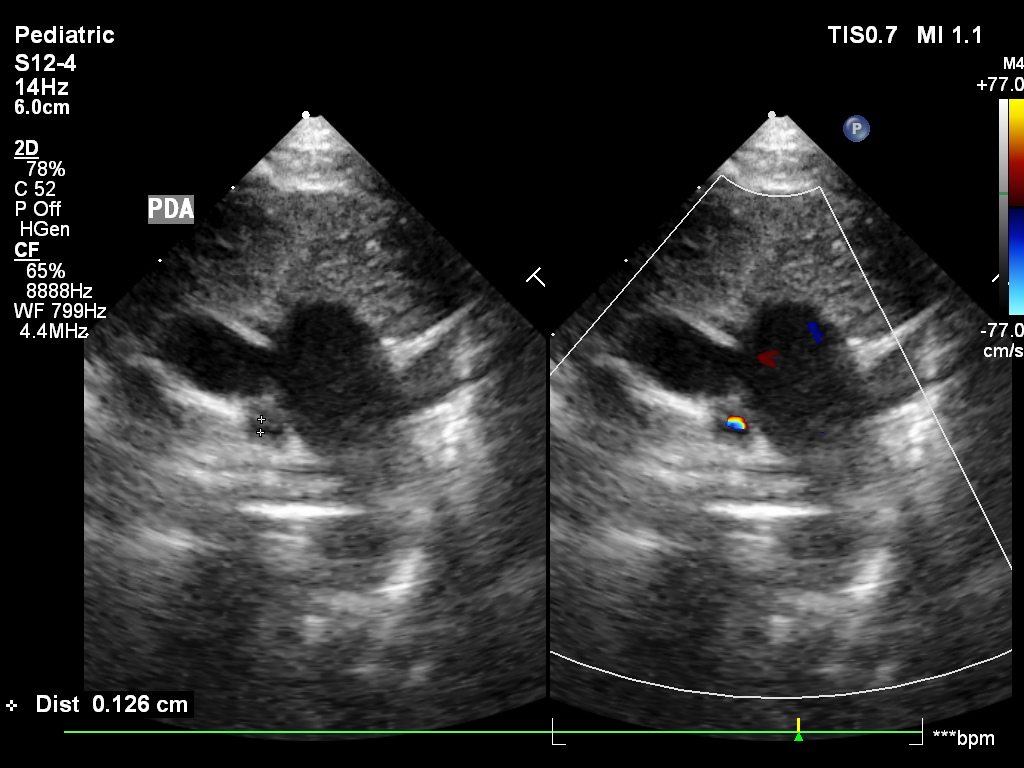
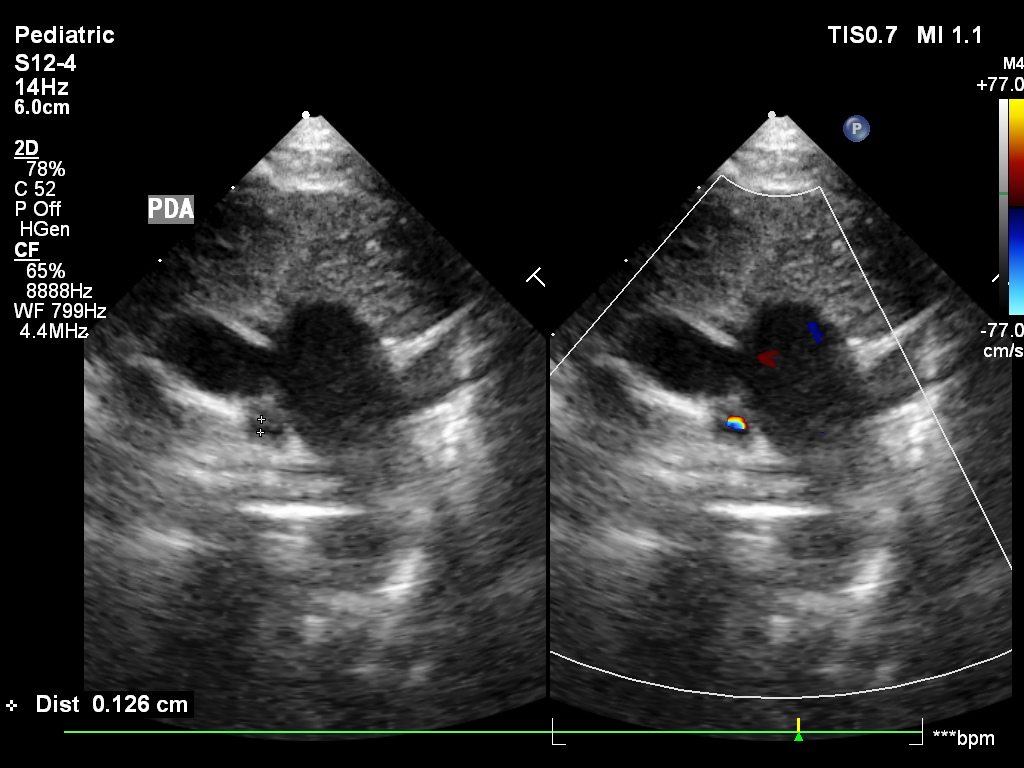
In the first patient, Transthoracic echocardiography showed tricuspid atresia with a smallish right ventricle, small ventricular septal defect, infundibular pulmonary stenosis, and stretched patent foramen ovale with bidirectional shunt mostly right to left shunt. In the second patient, showed mitral atresia with hypoplastic left heart, prolapse tricuspid valve with moderate to severe tricuspid regurgitation, and tiny patent ductus arteriosus with duct dependent physiology.
Relevant Catheterization Findings
Interventional Management
Procedural Step
The first patient was hospitalised for 4 days in our Pediatric Intensive Care Unit (PICU) before he was referred to a tertiary hospital to undergo Fontan Procedure. A multidisciplinary approach between the pediatrician and cardiologist such as hemodynamic stabilization, avoiding dehydration, and infection control were made and become our main focus in managing this patient before referring them to the tertiary hospital.
Case Summary
Both Tricuspid atresia and Mitral atresia were rare CHD. The differential mechanism between Tricuspid and Mitral atresia based on duct-dependent physiology affected the survival rate of this patient. Most infants with undiagnosed duct-dependent physiology with Hypoplastic Left Heart Syndrome die within the first two weeks of life, with an average age at death of 4.5 days. Infants with Tricuspid Atresia may survive until adulthood with comprehensive treatment. Early diagnosis using TTE may help in increasing the survival rate in the rural area.


