Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-092
Post TAVR VIV (3 Valves) and CABG Coronary Access to LCx With Tight Undilatable SVG-PDA Lesion Treated With Shockwave, Scoring Balloons and Rotational Atherectomy
By Jonathan Xinguo Fang
Presenter
Jonathan Xinguo Fang
Authors
Jonathan Xinguo Fang1
Affiliation
Henry Ford Health,USA, Hong Kong, China1,
View Study Report
TCTAP C-092
CORONARY - Complex and Higher Risk Procedures for Indicated Patients (CHIP)
Post TAVR VIV (3 Valves) and CABG Coronary Access to LCx With Tight Undilatable SVG-PDA Lesion Treated With Shockwave, Scoring Balloons and Rotational Atherectomy
Jonathan Xinguo Fang1
Henry Ford Health,USA, Hong Kong, China1,
Clinical Information
Patient initials or Identifier Number
LL 20798138
Relevant Clinical History and Physical Exam
68/Fe with PMHx of HTN, HLD, T2DM , CAD s/p CABG x3 (vein graft to PDA, vein graft to OM1, LIMA to LAD w/ Dr. Aranki 3/9/2006 at BWH), AS s/p AVR (23magna ThermaFix pericardial valve w/ Ascending aortic aneurysm s/p supracoronary ascending aorta replacement with size- 30 hemashield graft , PCI to SVG-PDA graft in 2011, VIV TAVR in 2015, VIVIV TAVR in 2021 c/b CAD s/p PCI to the RCA. Now present worsening dyspnoea and chest pain.
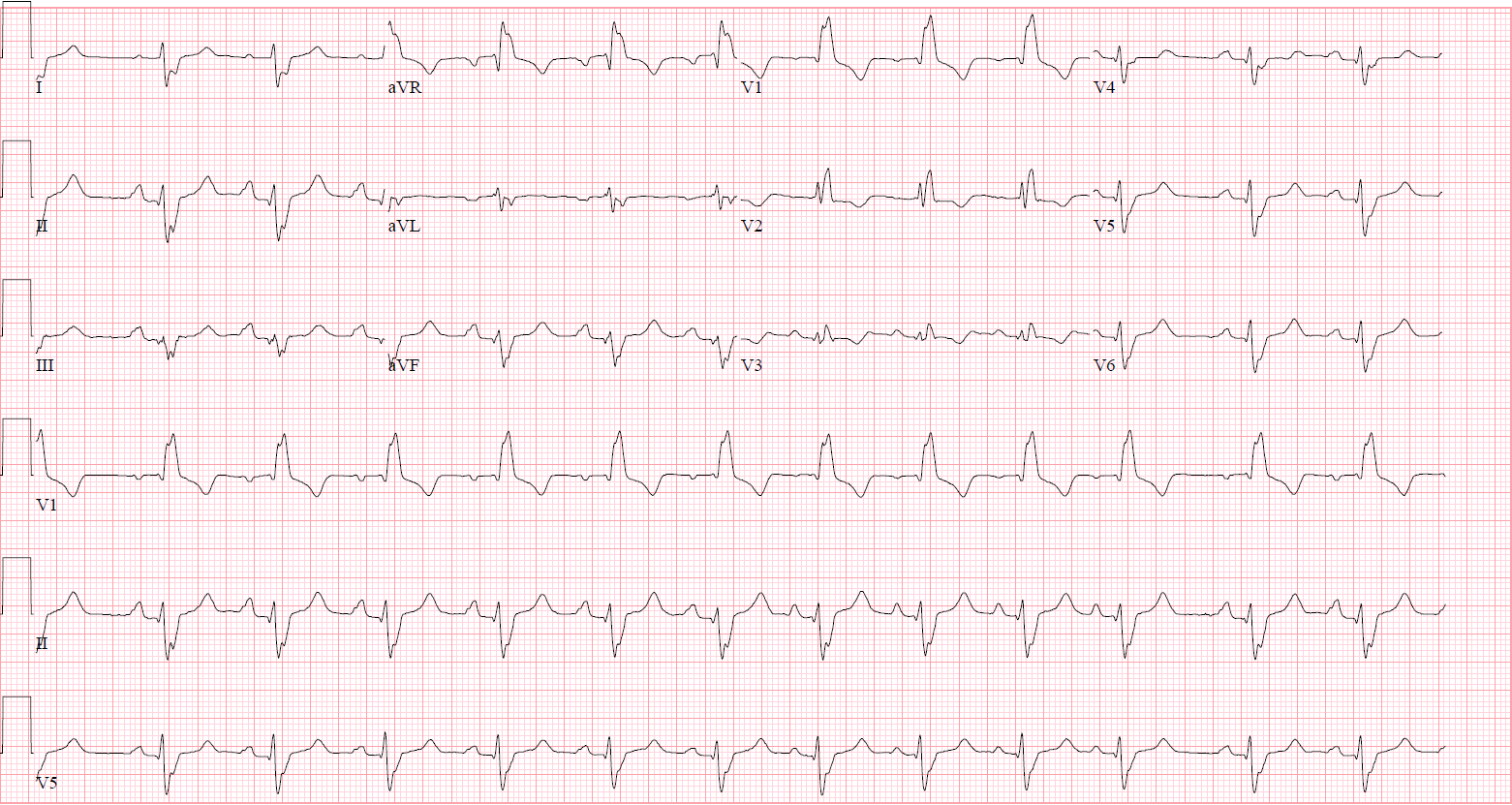
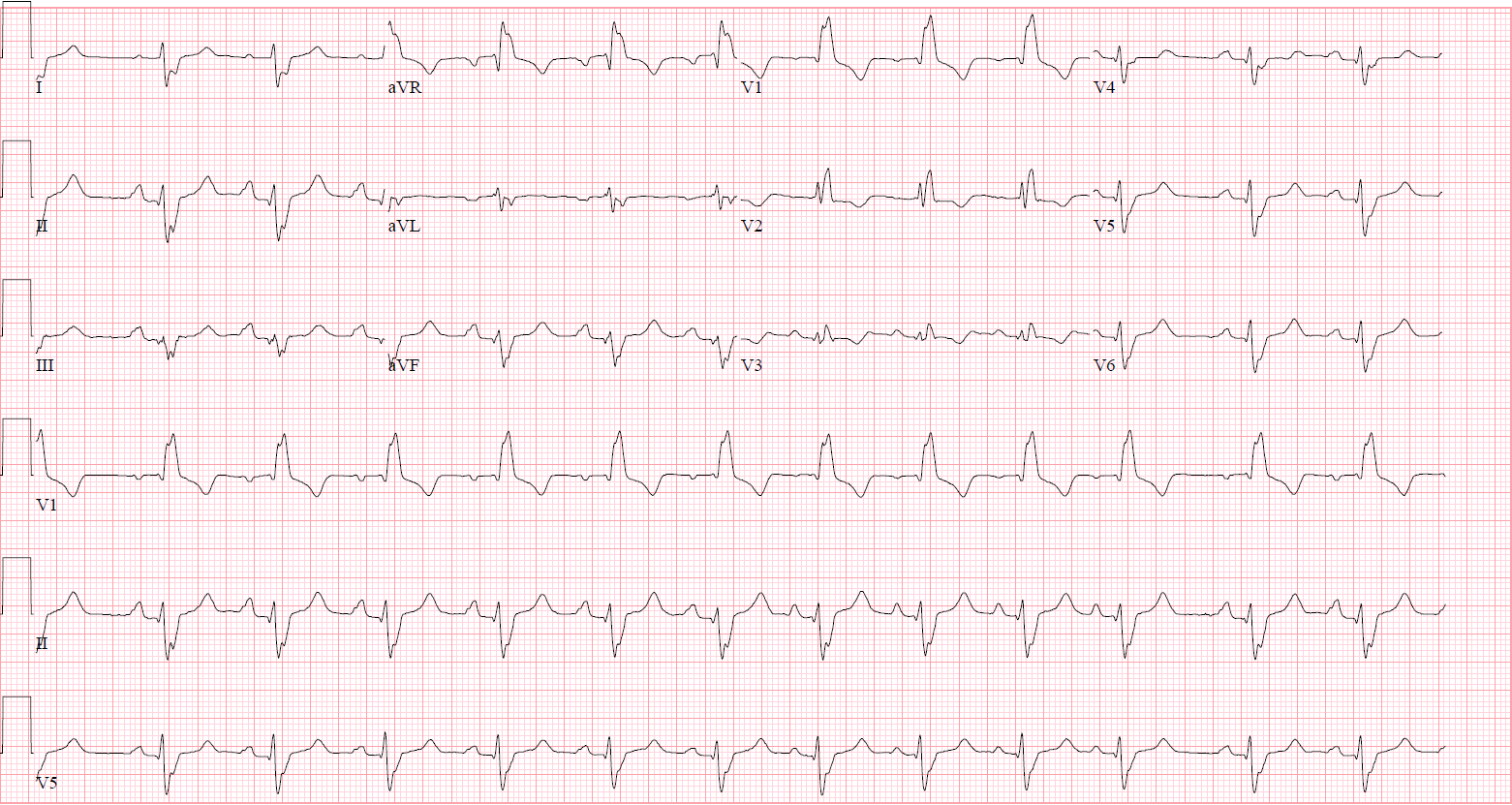
Relevant Test Results Prior to Catheterization
ECG showed RBBB, no dyanmic changeTroponin was not elevated Echocardiogram showed normal AV gradient and normal EF
Relevant Catheterization Findings
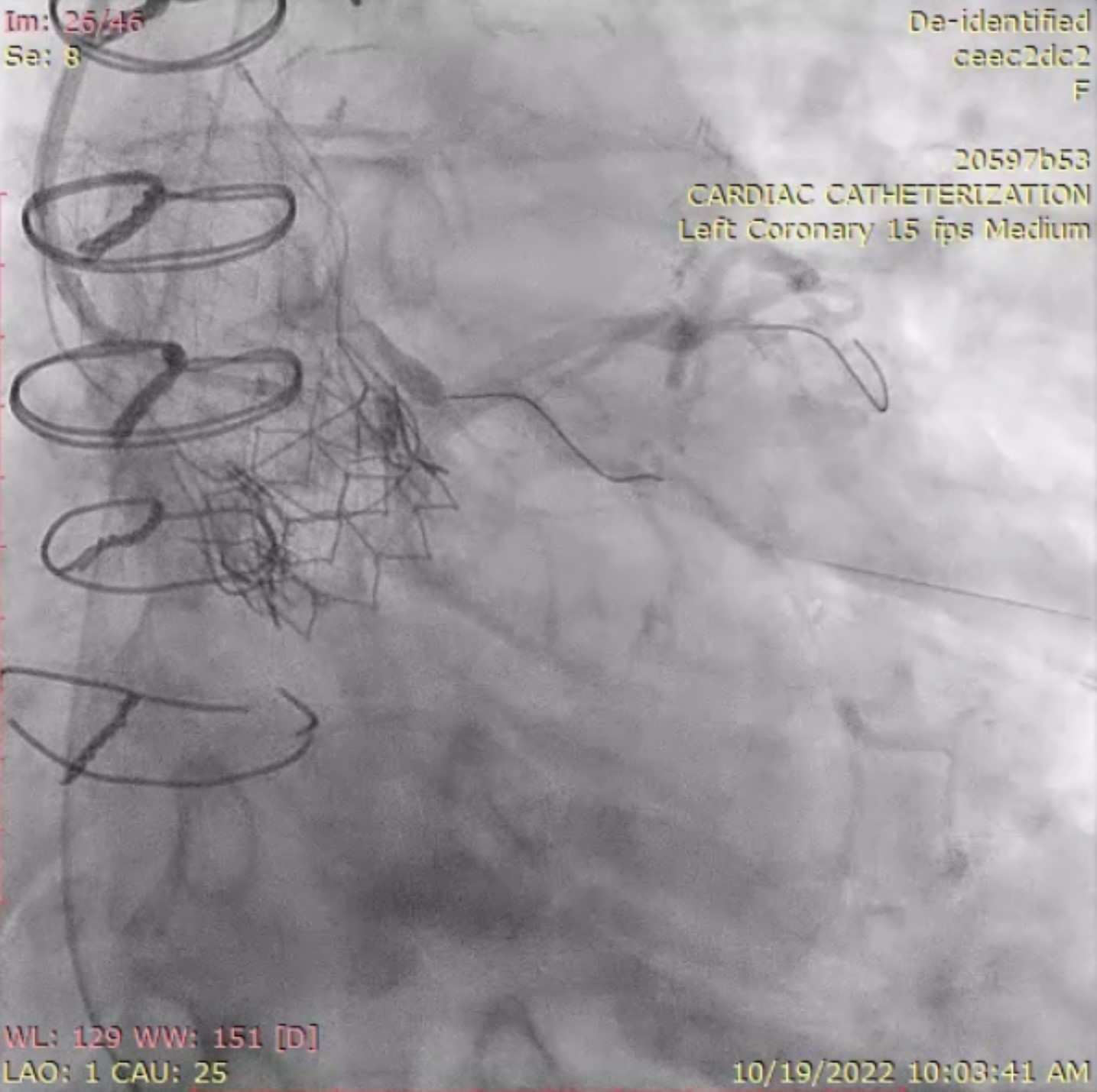
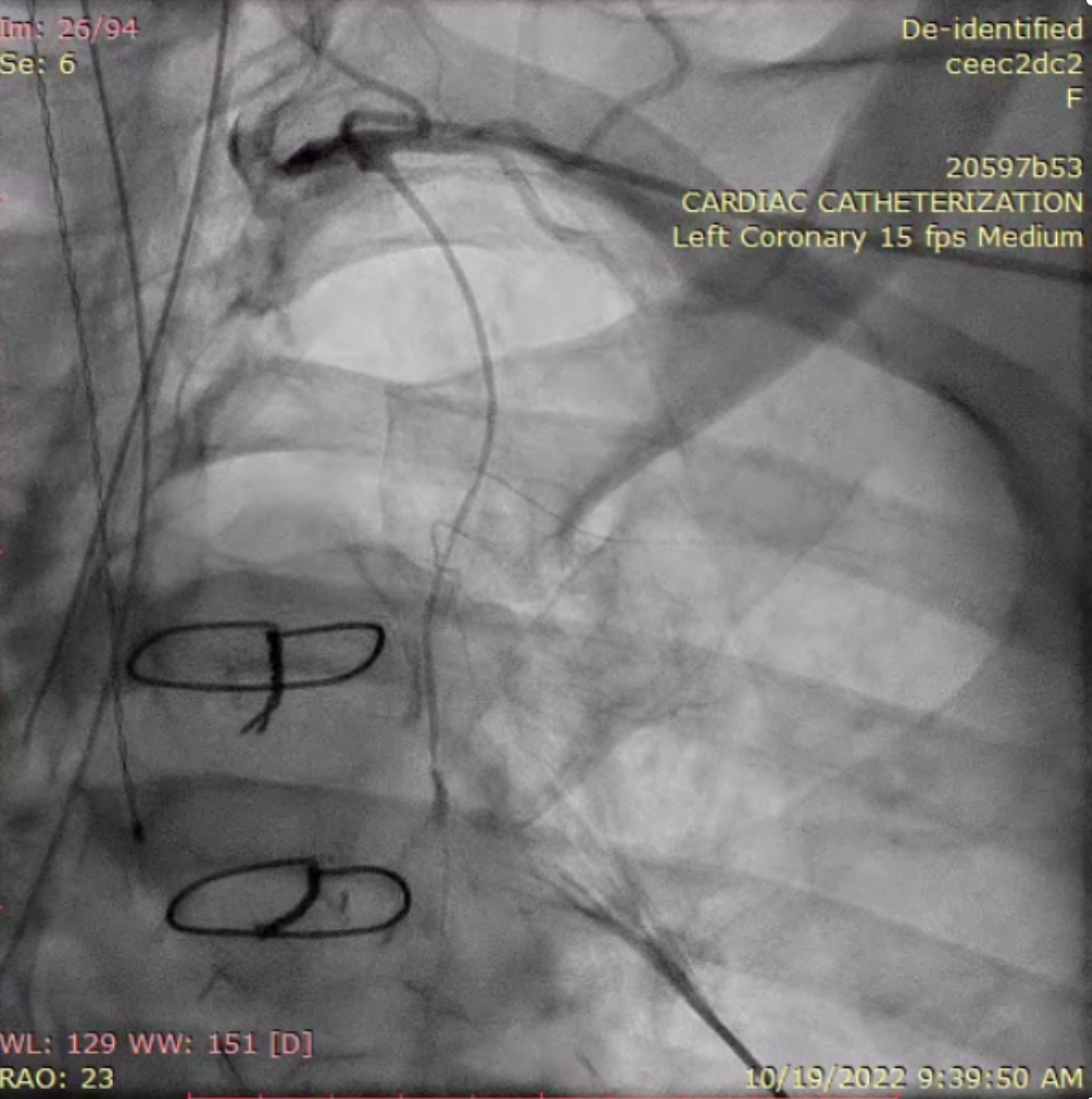
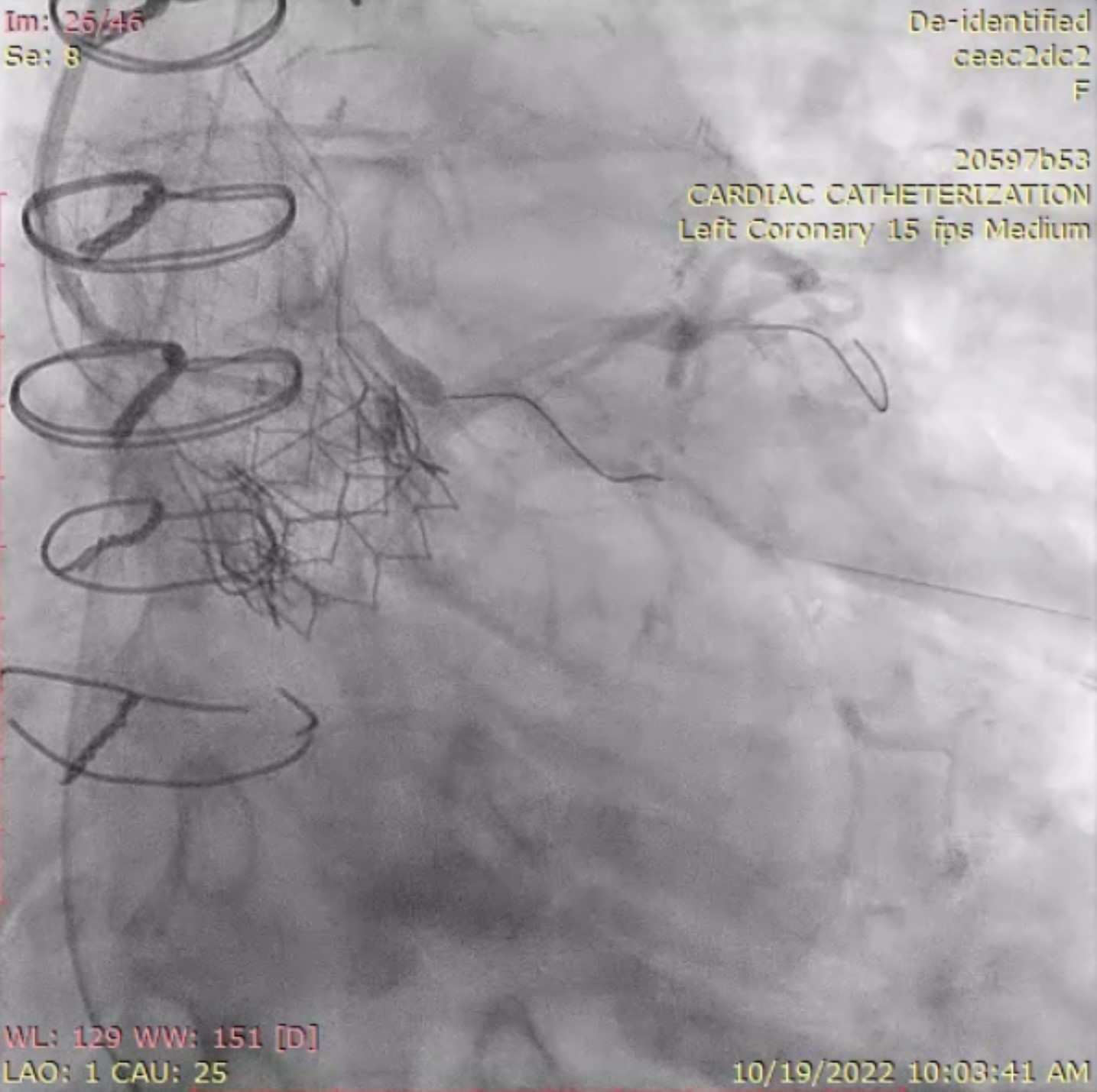
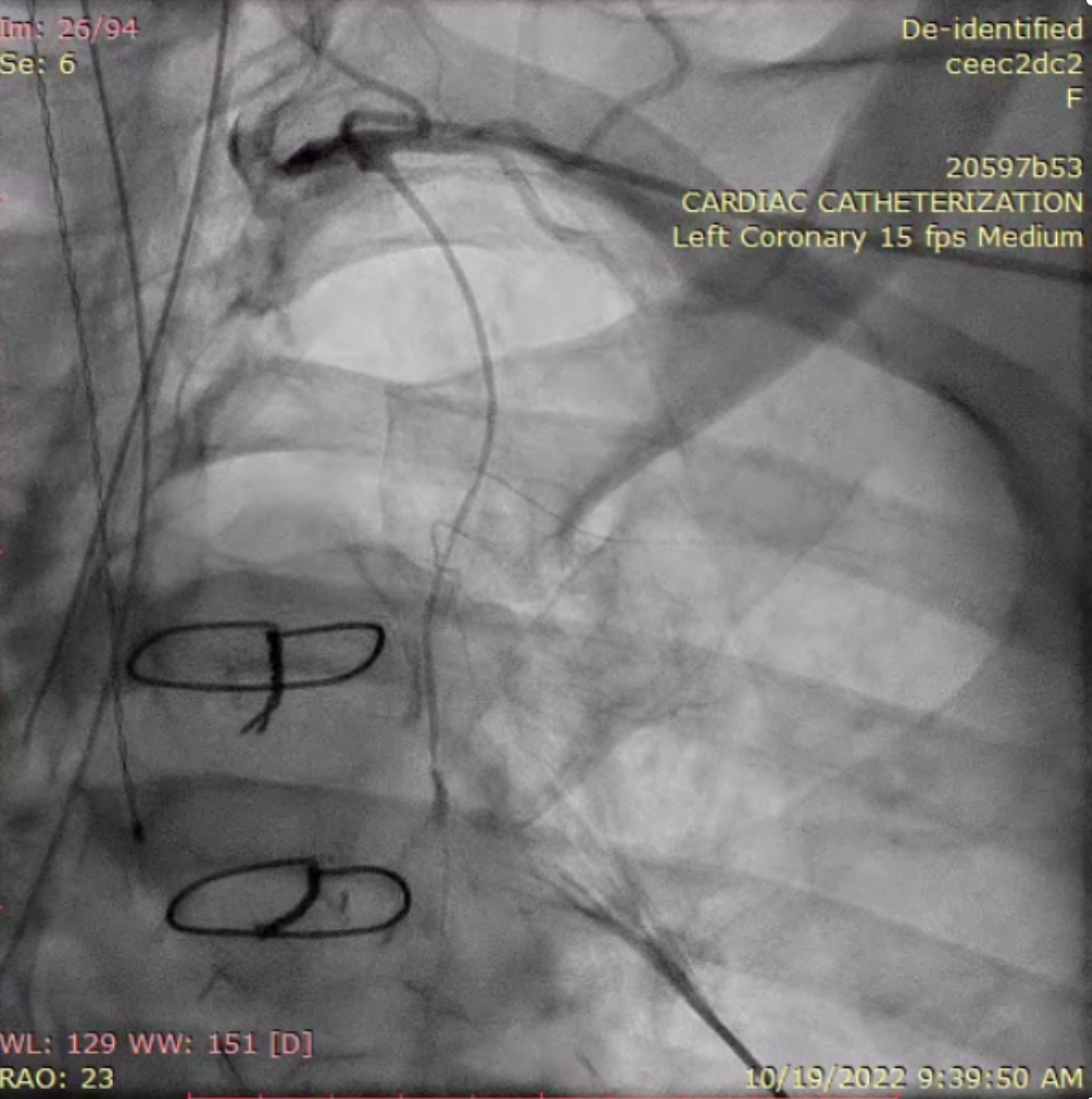
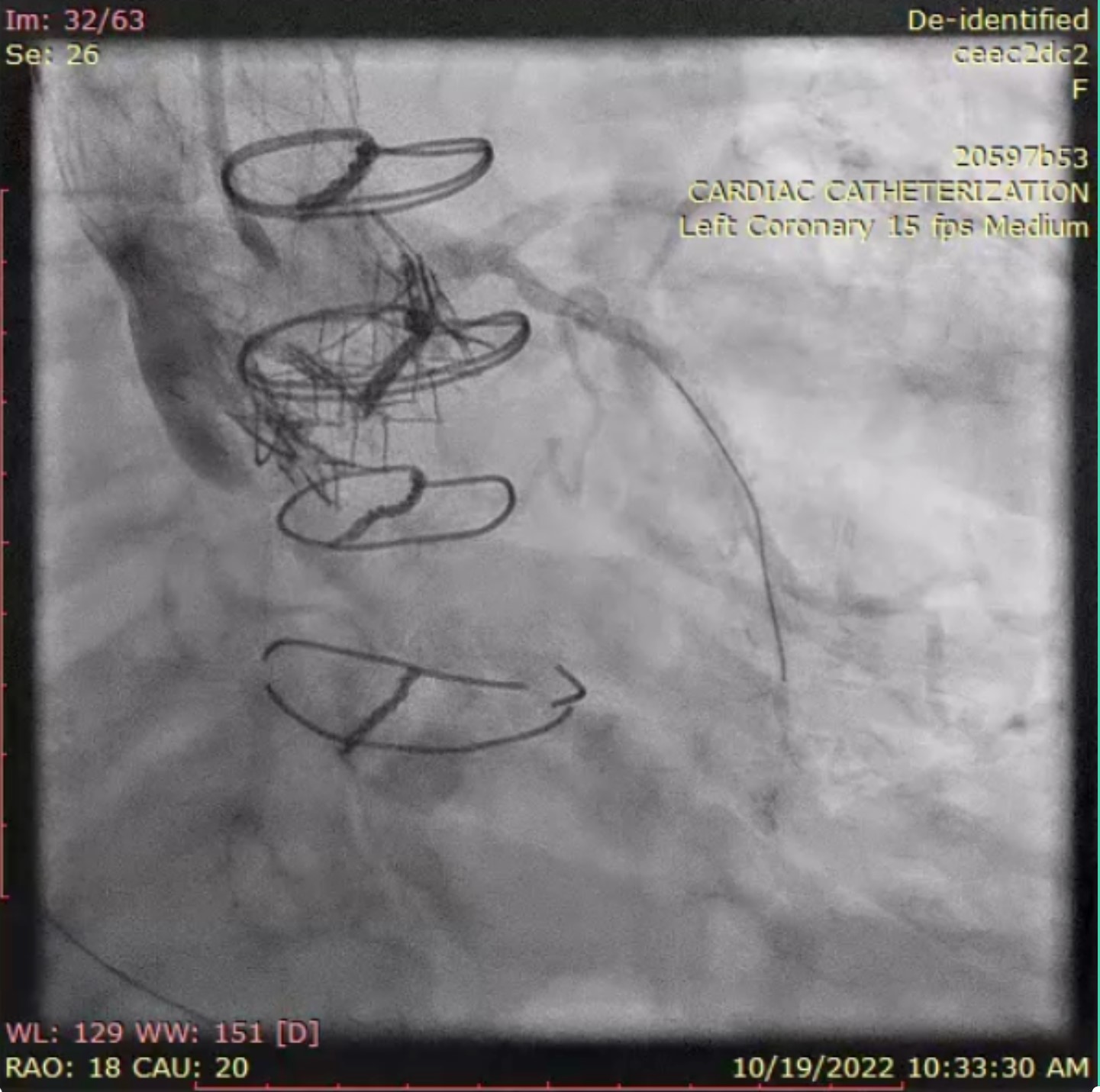
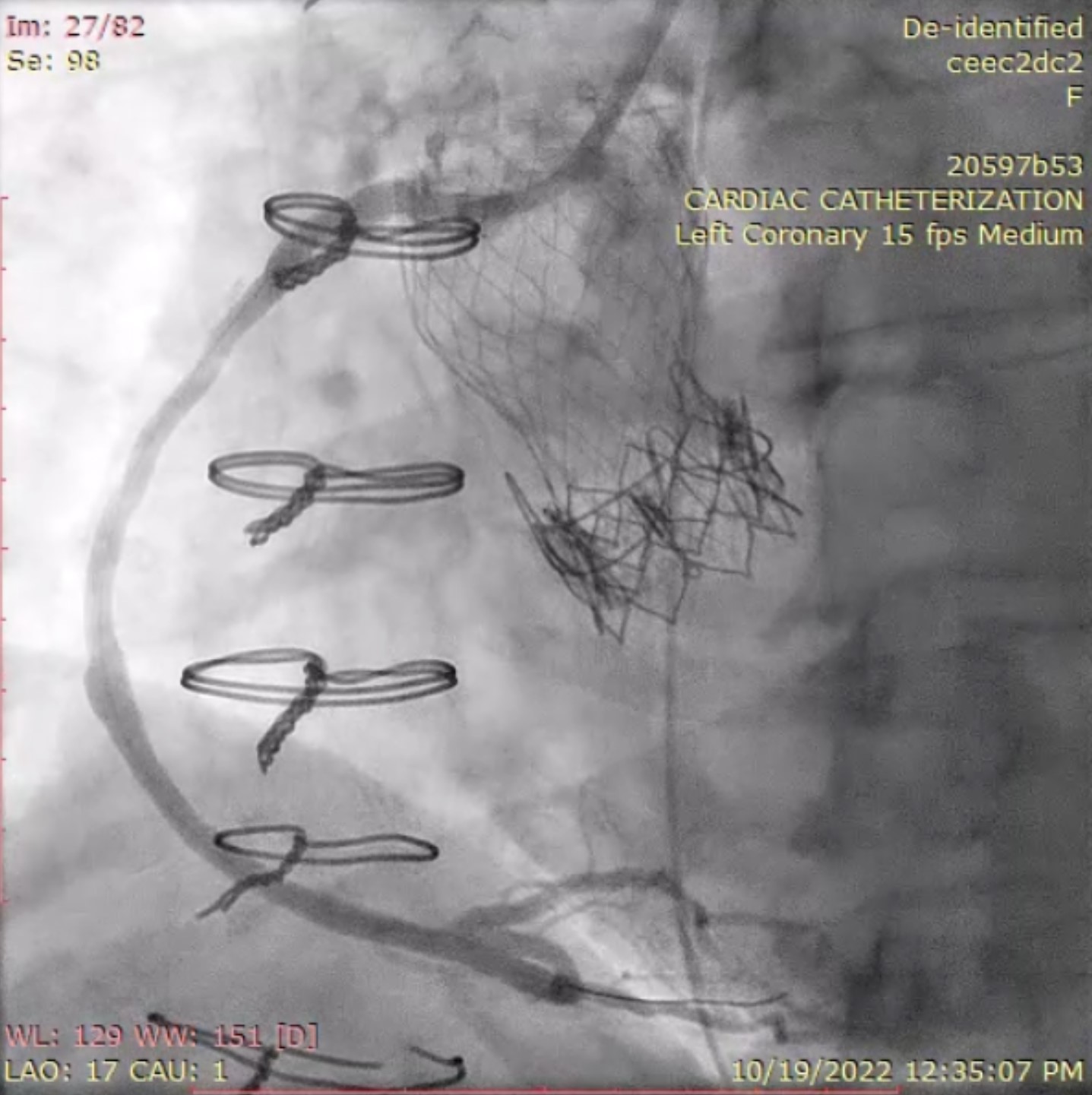
Coronary angiogram showed 90% disease LIMA, native LAD moderate. mLCx 80% disease. SVG-PDA graft ostial stent 90% ISR


Interventional Management
Procedural Step
There was difficulty in engaging the left coronary system. A 7Fr JR4 guide was used via a left radial approach in the aorta with a minamo wire sent into the LAD for stabilization. A turnpike LP with a BMW wire exchanged to a pilot 50 crossed the LCx into distal OM and de-escalated back to BMW. The LCx lesion was treated with 2.5 SC balloon, 2.5x38 DES and 2.5 NC balloon.
The SVG to RPDA graft ostium was at the upper margin of the TAVR valve frame with severely calcified ostial ISR and was difficult to engage. We switched to right femoral access owing to radial spasm and engaged the SVG graft with a 7Fr JR4. We treated the lesion sequentially with 3.5 angiosculpt, 4.0 shockwave lithotripsy, 4.0 scoreflex, 1.4 laser atherectomy at 60/40, then rotational atherectomy with 1.75 burr at 200kRPM and finally 4.0 NC in order to achieve adequate expansion. A 4.0x24 Megatron DES. was deployed followed by 4.0 NC postdilation. Good angiographic result was achieved. Eagle-eye IVUS did not cross.

Case Summary
Successful PCI to OM via difficult-to-engage LMCA post TAVI ViViV. Successful PCI to ostial SVG-OM1 undilatable lesion with Shockwave, NC, scoring balloon, laser atherectomy and rotational atherectomy.This case demonstrates successful intervention in a difficult-to-engage post ViV TAVR coronary and also complex intervention of an SVG-PDA graft with off-label use of atherectomy with good result


