Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-096
When a Stent Was Left Behind..
By Emma Yaakop, Farook Ahmad, Chandan Deepak Bhavnani, Chan Meei Wah, Faizal Khan Bin Abdullah, Asri Ranga
Presenter
Chandan Bhavnani
Authors
Emma Yaakop1, Farook Ahmad2, Chandan Deepak Bhavnani1, Chan Meei Wah1, Faizal Khan Bin Abdullah3, Asri Ranga3
Affiliation
Hospital Serdang, Malaysia1, Colchester Hospital, United Kingdom2, Sultan Idris Shah Serdang Hospital, Malaysia3,
View Study Report
TCTAP C-096
CORONARY - Complications (Coronary)
When a Stent Was Left Behind..
Emma Yaakop1, Farook Ahmad2, Chandan Deepak Bhavnani1, Chan Meei Wah1, Faizal Khan Bin Abdullah3, Asri Ranga3
Hospital Serdang, Malaysia1, Colchester Hospital, United Kingdom2, Sultan Idris Shah Serdang Hospital, Malaysia3,
Clinical Information
Patient initials or Identifier Number
IM
Relevant Clinical History and Physical Exam
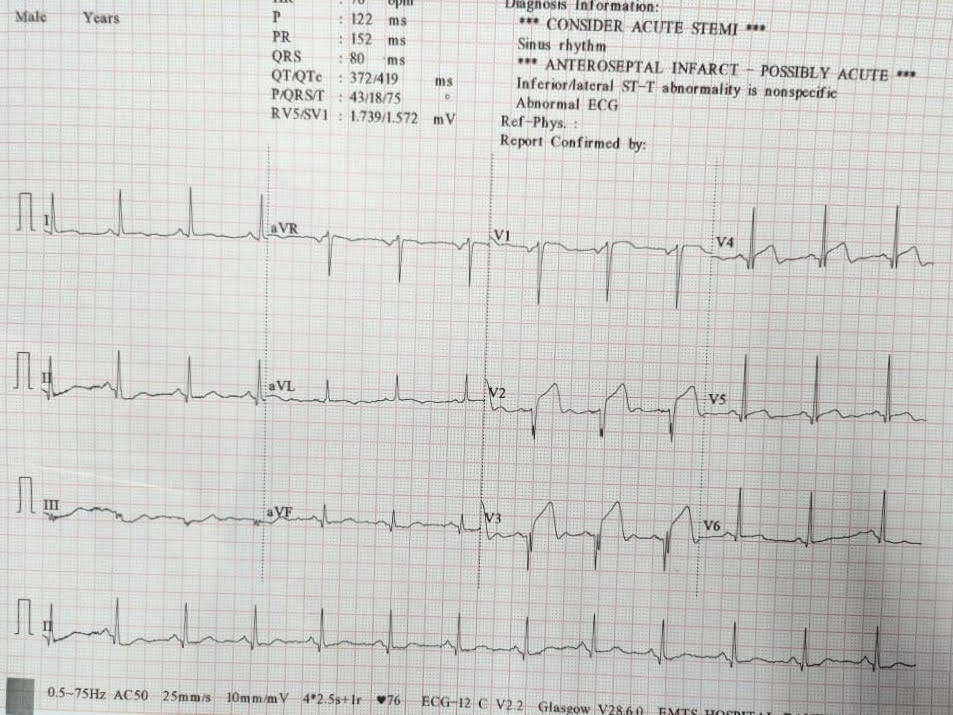
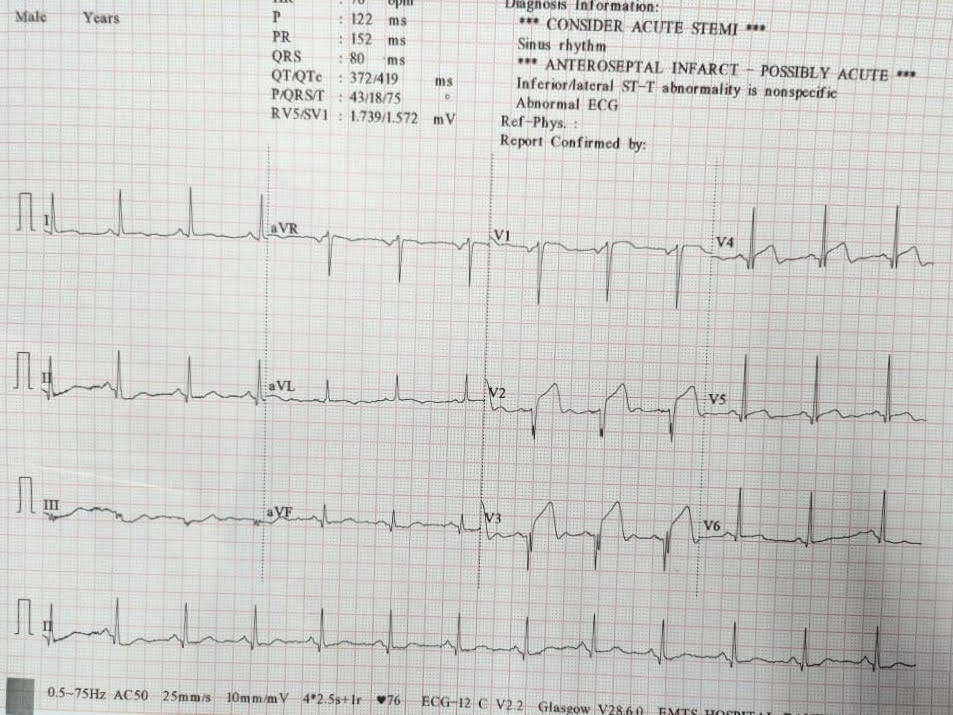
A previously fit 44-year-old gentleman, also an active smoker, presented to a district general hospital (DGH) with cardiac chest pain for 3 days duration. ECG on arrival at DGH showed ST segment elevation at lead V2-V3 and reciprocal changes in inferior leads indicating anteroseptal STEMI. As he was pain free on arrival to DGH, he was started on dual anti platelet and anticoagulant but not thrombolysis therapy. He was then referred to our cardiac centre for early invasive coronary intervention.
Relevant Test Results Prior to Catheterization
Total white blood cells 11.0 x109/L, Haemoglobin 15.7 g/dL, Platelet 345 x109/L, Troponin I 13,028 ng/L, Urea 3.5 mmol/L, Sodium 138 mmol/L, Potassium 3.8 mmol/L, Creatinine 81 umol/L, INR 1.04, Total cholesterol 7.84 mmol/L, Triglycerides 1.30 mmol/L, LDL 6.49 mmol/L, HDL 0.75 mmol/L. Echocardiogram showed ejection fraction 50% with mild hypokinesia at LAD territory. Electrocardiogram showed sinus rhythm with ST segment elevation at lead V2-V3 and reciprocal changes in inferior leads.
Relevant Catheterization Findings
Coronary angiogram showed dominant Right Coronary Artery (RCA) with 70 – 80% stenotic lesion from proximal to mid RCA and triple vessel disease with left main (LM) stem lesion. The details are as follows; 50-60% stenosis of distal occlusion of left main stem, 90% stenosis at ostial LAD, 90%stenosis at proximal LAD and 70% stenosis at mid LAD 70%. Only mild lesion was found in Left circumflex (LCx).
Interventional Management
Procedural Step
Coronary angioplasty was performed via right radial access with guiding catheter Extra Back Up 3.0 / 6Fr with workhorse wire run-through floppy coronary down into LAD.LAD was pre-dilated with semi-compliant (SC) balloon 2.0x15mm. Intravascular ultrasound (IVUS) findings revealed vessel size with minimal luminal area (MLA) mid LAD 3.0mm2, proximal LAD 3.5mm2 and LM 4.0-4.5mm2, further preparation was performed with non-compliant (NC) balloon 3.0x15mm, then stenting of mid to proximal LAD with drug eluting stent (DES) 3.0x40mm and proximal LAD to LM with another DES 3.5x30mm. Post dilatation was done with NC balloon 3.0x15 mm and 3.5x15 mm, and post dilatation of LM to proximal LAD with NC balloon 4.0x15 mm, all at high pressure.Sudden total occlusion of LCx with coronary blood flow TIMI 0 occurred, possibility of plaque shift or dissection whilst second workhorse coronary wire was wired down to LCx and good TIMI 3 coronary flow achieved with SC balloon with 2.0x15 mm. T and protrusion (TAP) stent strategy was attempted with DES 2.5x18mm into ostial LCx, however wire was lost while the DES unfortunately dislodged and stuck into the LM.Cullote stenting was applied via Double kissing (DK) balloon strategy with NC balloon 3.5x15mm into LAD and NC balloon 2.5x5mm into LCx and the LCx was pre-dilated with cutting balloon 3.0x15mm.
 Fig 678 TCTAP.pptx
Fig 678 TCTAP.pptx
Case Summary
Plaque shift is known as one of the complications due to side branch occlusion following PCI in coronary bifurcation lesions. In this case, we demonstrated two strategies to overcome this phenomenon with TAP stent and cullote stent technique for optimization of SB stenting. While TAP stenting is the recommended strategy of provisional SB stenting, this technique can result in gap, protrusion into the main branch or stent distortion within the side branch. On the other hand, DK-culotte stenting is a feasible technique in order to achieve optimal and complete coverage of the side branch, also in managing complications as ostial LCx dissection in LM bifurcation lesion.


