Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-135
The Bad, the Ugly and the Good.
By Jayakumar Mohanaraj, Houng Bang Liew
Presenter
Mohanaraj Jayakumar
Authors
Jayakumar Mohanaraj1, Houng Bang Liew2
Affiliation
Ministry of health Malaysia, Malaysia1, Queen Elizabeth II Hospital, Malaysia2,
View Study Report
TCTAP C-135
CORONARY - Drug-Eluting Balloons
The Bad, the Ugly and the Good.
Jayakumar Mohanaraj1, Houng Bang Liew2
Ministry of health Malaysia, Malaysia1, Queen Elizabeth II Hospital, Malaysia2,
Clinical Information
Patient initials or Identifier Number
Mr. KA
Relevant Clinical History and Physical Exam
Patient is a 50 years old farmer. He is a smoker with no known medical illness. He presented with chest pain while farming. He was brought by family to a district hospital 2.5 hours away from a PCI center. ECG showed acute LMS syndrome. He was thrombolysed and started on noradrenaline support as BP was low 80/50 mmHg. Post thrombolysis, inotropes reducing and pain score improved. He was then transferred over to our center for urgent coros and PCI.
Relevant Test Results Prior to Catheterization
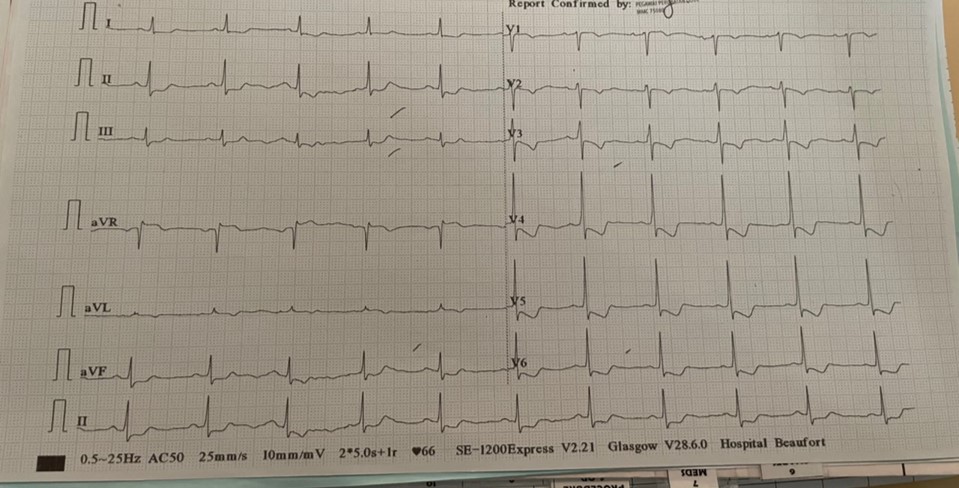
His blood parameters prior to catheterization was normal including the renal profile.All peripheral pulses were palpable.Chest X-ray showed no widened mediastinum or any infective changes and no pulmonary infiltrations as well.ECG prior catheterization as below.


Relevant Catheterization Findings
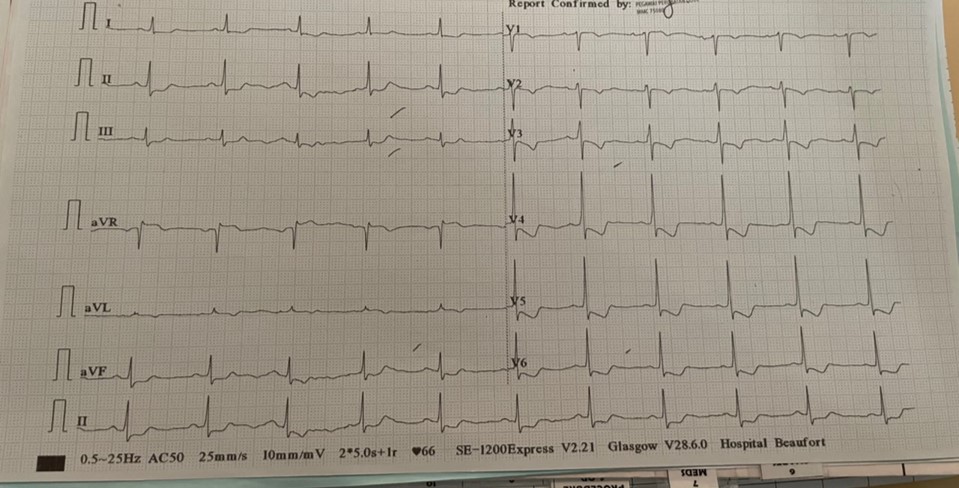
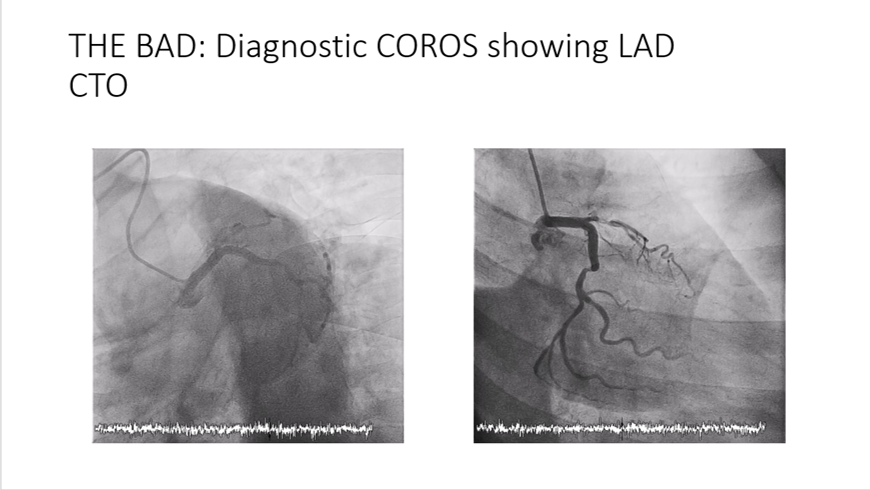
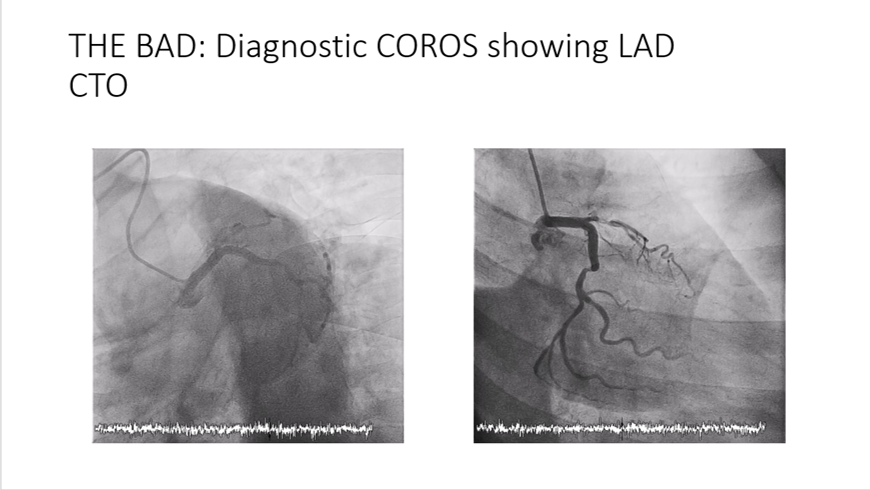
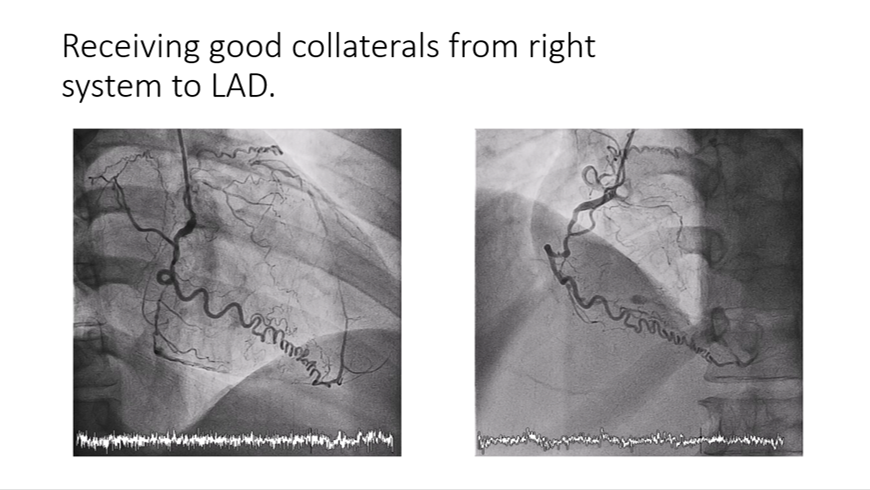
Proceeded with coros which showed CTO from ostial LAD, 80-90% disease of proximal LCx and midsegment CTO of RCA which also supplies collaterals to LAD. Discussion with patient on table done regarding CABG vs high risk PCI and he opted for PCI as he is the sole breadwinner of his family and he has young children. Decision was conveyed to family.
Interventional Management
Procedural Step
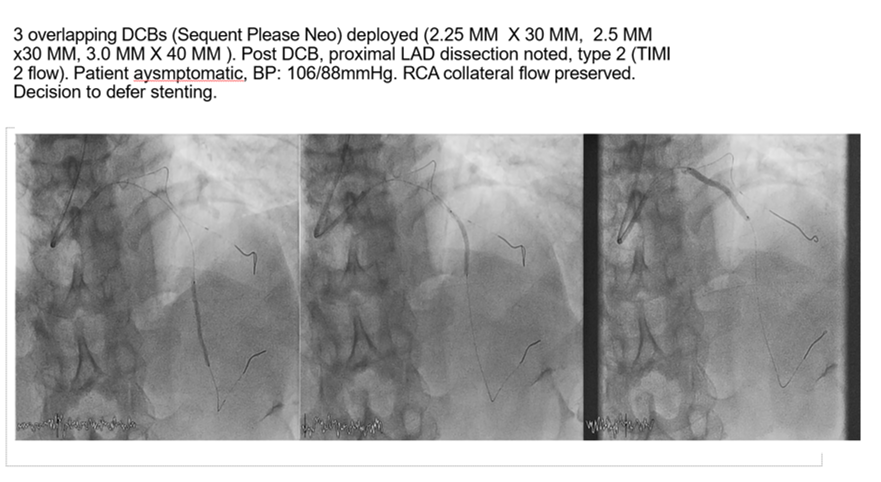
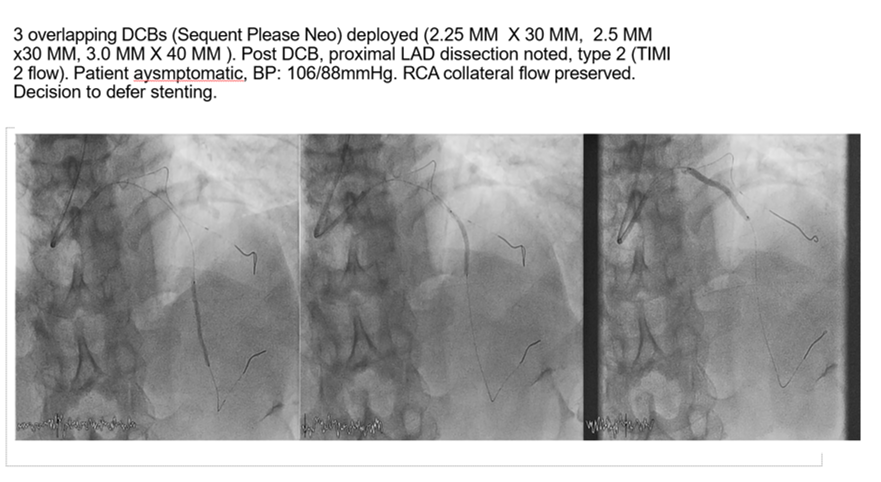
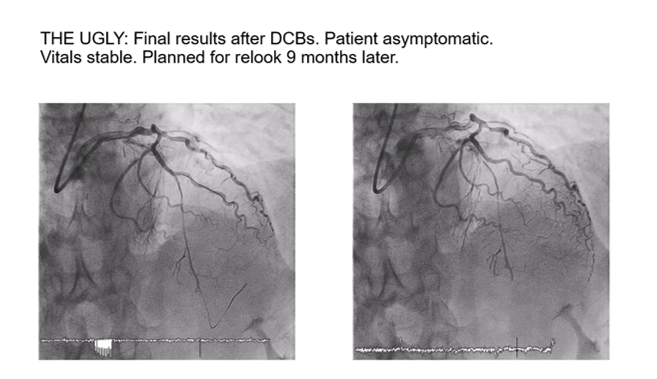
EBU 3.5GC used to engage the LCA. Pilot 50 wire used to attempt the ostial LAD CTO but GC was being kicked out, BMW used to wire the LCx for extra support. Second puncture made to RFA for collaterals injection. Able to cross after multiple attempts to a diagonal branch with 1.0mm balloon support. Pre-dilatation performed with 1.0mm balloon at proximal lesion, then wire was able to advance to distal LAD. Confirmed with collaterals injection. Then, pre-dilatation performed sequentially, initially with a 1.0mm balloon then with 2.0mm and 2.5mm balloons. No antegrade flow achieved. Collaterals injection showed good retrograde flow and fenestrations made over the winged balloon for contrast injection to ascertain the flow pattern. Decided to perform 3 minutes inflation x 3 from distal to proximal with a 3.0 NC Trek balloon. Noted antegrade flow achieved and dissection at proximal LAD and there was competitive flow from RCA collaterals. As we saw good lesion vessel pre-dilatation we decided to treat the vessel with three DCBs Sequent Please Neo, 2.25mm x 30mm distally, 2.5mm x 30mm midsegment and from ostial 3.0mm x 40mm. However, final results were ugly but patient was stable with no chest pain and hemodynamically stable. We decided to relook this patient 6-9 months later and stage to LCx and RCA. Patient has been well and back to farming since procedure and asymptomatic. He came back for relook 9 months later and we saw positively remodeled LAD with healed dissection at proximal.
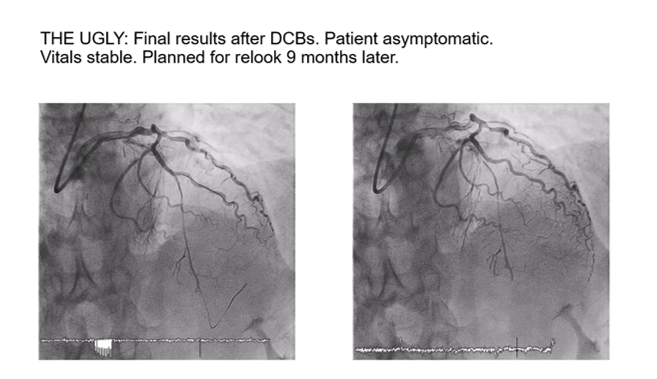
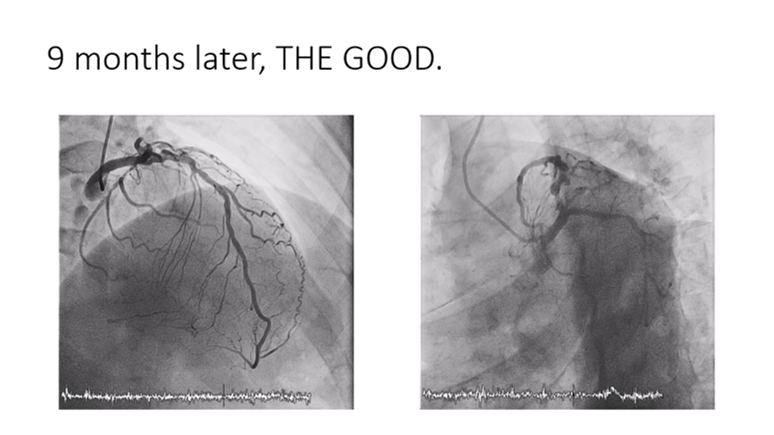
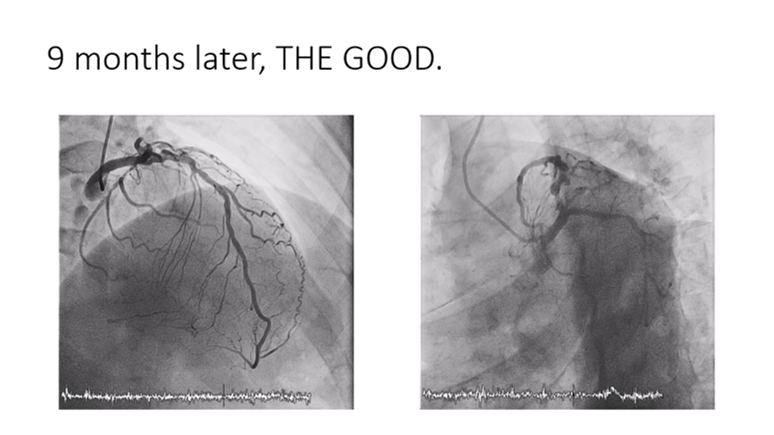
Case Summary
Here, we would like to conclude that DCBs work with CTO as well and this is not the first case we have treated with DCBs. Even though there was dissection at first, we have showed that it will heal even with DCBs. In our case, we managed to leave no metal behind as he is still relatively young and DCBs are cost effective and also helps in situations like ours where the patient comes from a poor socio-economic status and if he defaults follow ups or medications, he may come back with ISR or stent thrombosis in future if stents were deployed instead.


