Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-166
To Stent or Not to Stent? Imaging and Physiology Guided Percutaneous Coronary Intervention in Acute Myocardial Infarction
By Aldreus Calabia, Conrad Estanislao, Rodney Montesino Jimenez
Presenter
Aldreus Calabia
Authors
Aldreus Calabia1, Conrad Estanislao1, Rodney Montesino Jimenez1
Affiliation
St. Luke's Medical Center, Philippines1,
View Study Report
TCTAP C-166
IMAGING AND PHYSIOLOGIC LESION ASSESSMENT - Physiologic Lesion Assessment
To Stent or Not to Stent? Imaging and Physiology Guided Percutaneous Coronary Intervention in Acute Myocardial Infarction
Aldreus Calabia1, Conrad Estanislao1, Rodney Montesino Jimenez1
St. Luke's Medical Center, Philippines1,
Clinical Information
Patient initials or Identifier Number
J.M
Relevant Clinical History and Physical Exam
51-year-old male, smoker and dyslipidemic. 9 hours prior, complained of intermittent chest discomfort hence was brought to ER. Upon arrival, chest pain was partially resolved even without any intervention. On PE, He was awake, blood pressure of 110/70 mmHg with bradycardia of 55 bpm, breath sounds were clear, heart rhythm was regular with no appreciable murmurs, apex beat was at the 5th ICS mid-axillary line, pulses were full and equal.
Relevant Test Results Prior to Catheterization
ECG 12 leads: 1 mm ST segment elevation in leads II, III, and AvF with no reciprocal changes. Serial ECG done 1 hour and 3 hours after have the same findings with no dynamic or evolution changesChest x-ray: NormalHS Troponin I: 653 ng/LCreatinine: 1.09 mg/dLNa: 147 mEq/LK: 4.5 mEq/L2d echo: Normal left ventricular diameters with regional wall motion abnormality involving the inferior and inferolateral segments. EF of 43.1% by Simpson’s method. Grade 1 left ventricular diastolic dysfunction
Relevant Catheterization Findings
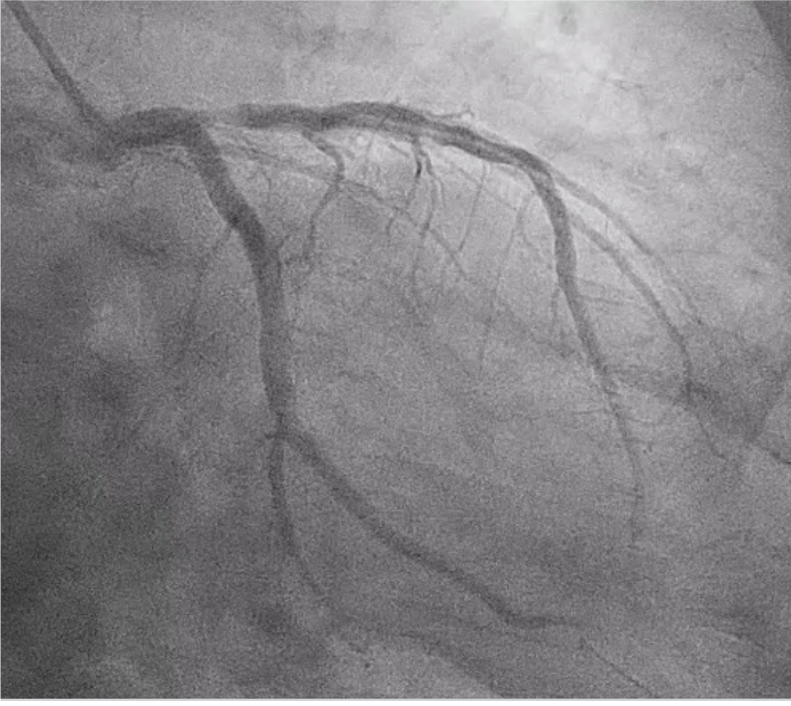
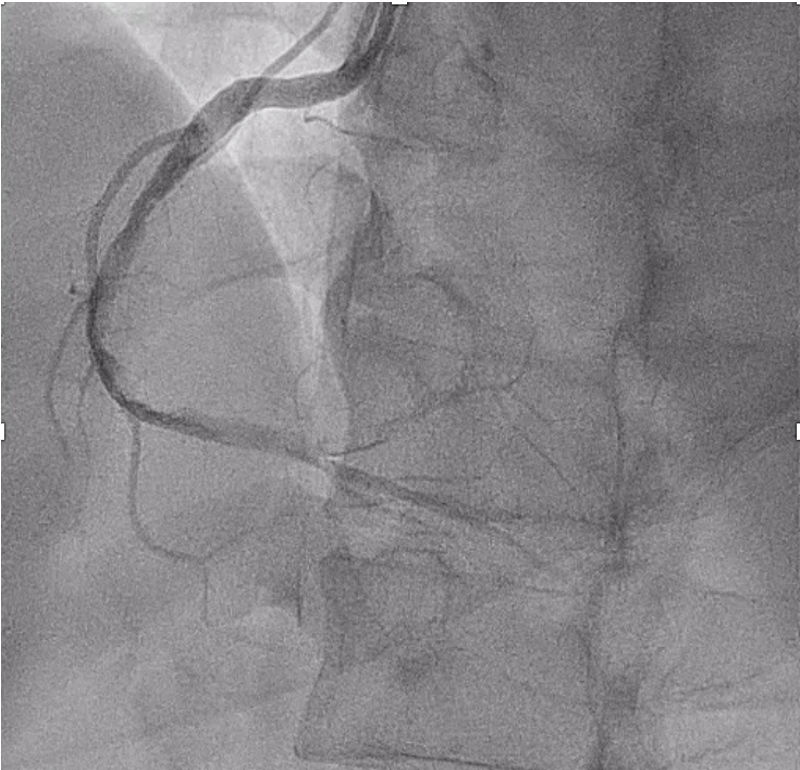
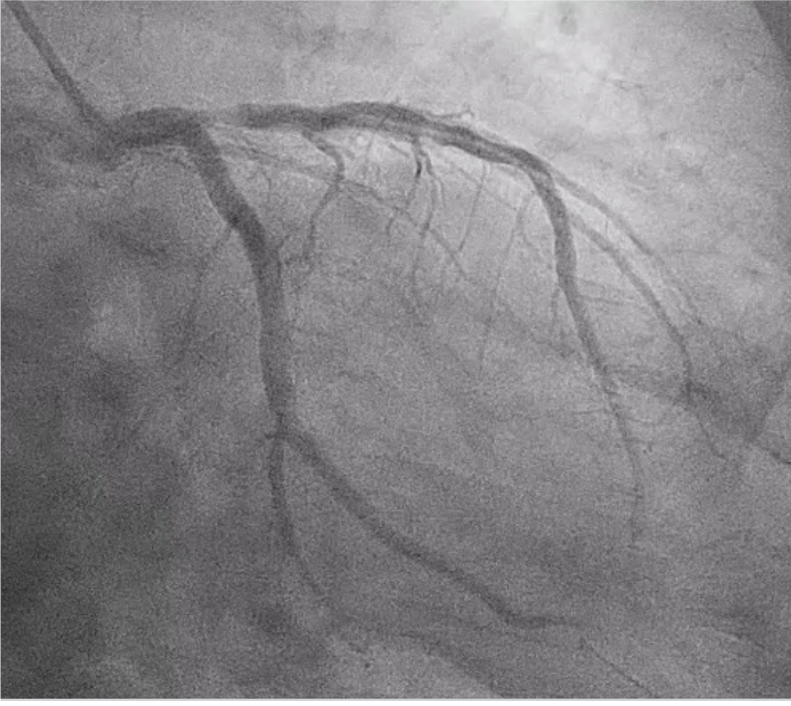
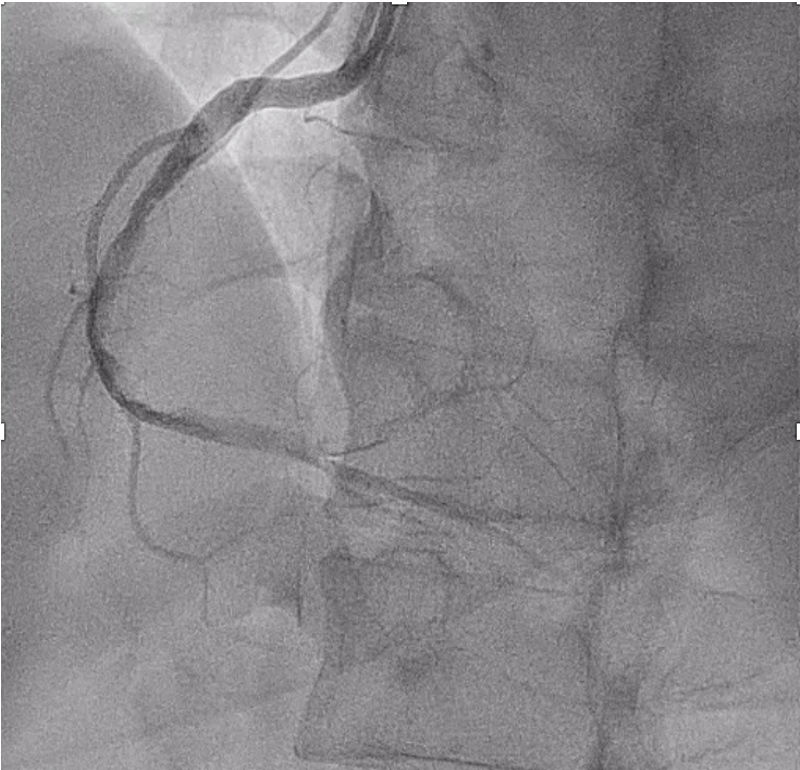
Left main coronary artery appears disease free. LAD is a type 3 vessel with severe stenosis (80%) of the ostium with TIMI 2 flow. LCx appears disease free. RCA is a co-dominant vessel with thrombus from the proximal segment to the right posterolateral ventricular branch with TIMI 2 flow.
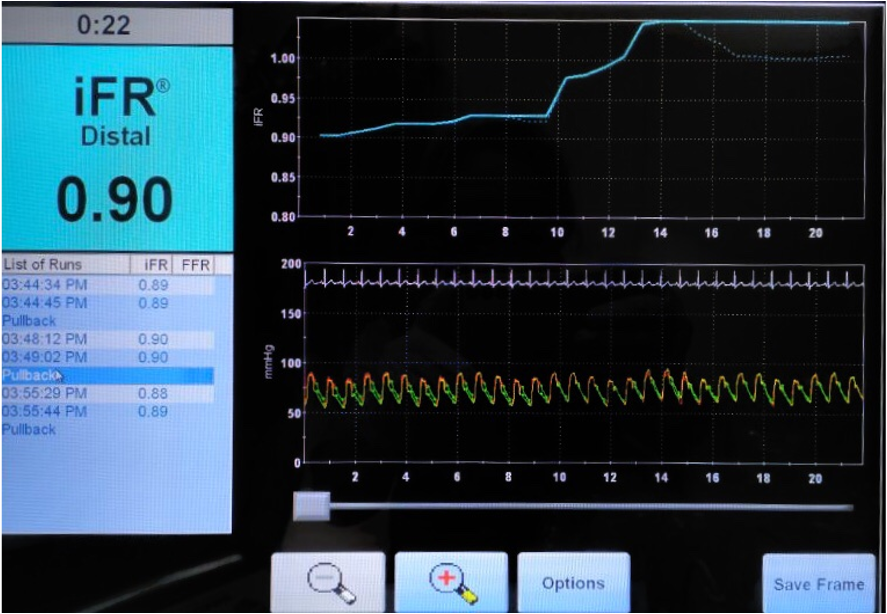
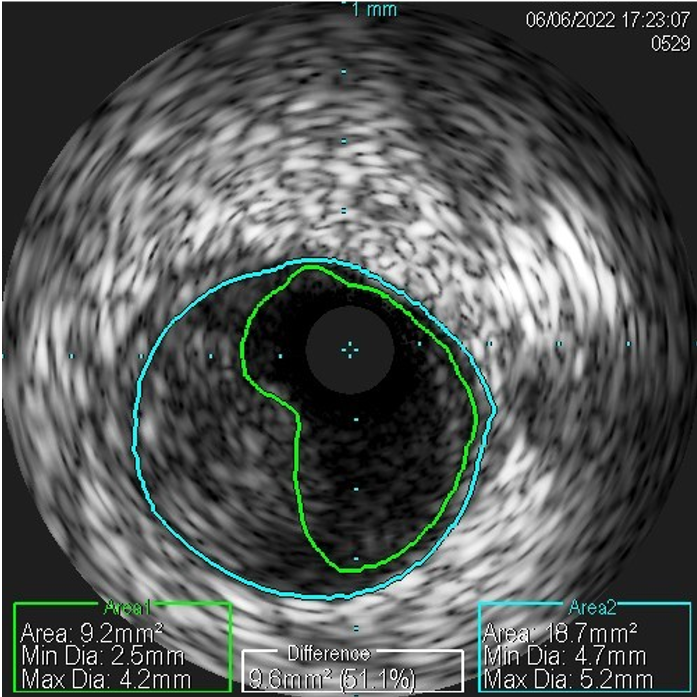
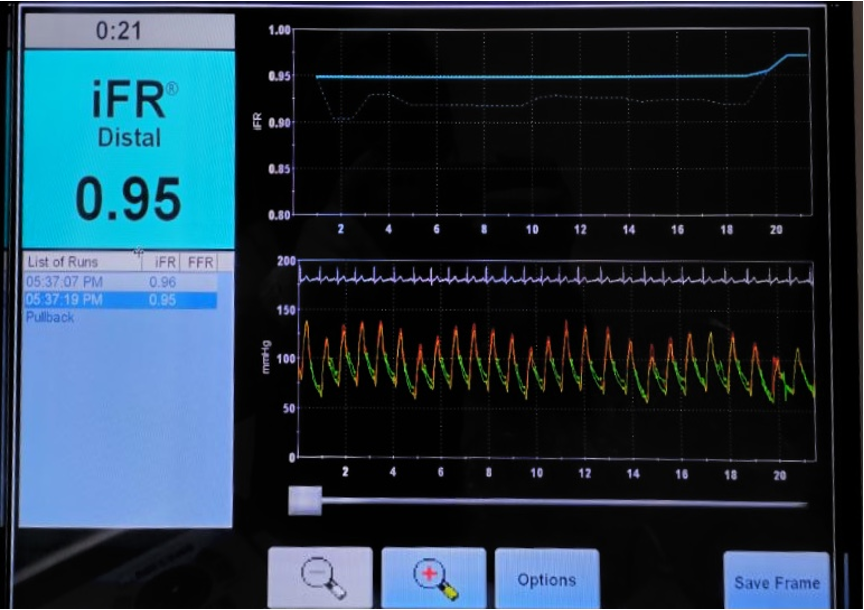
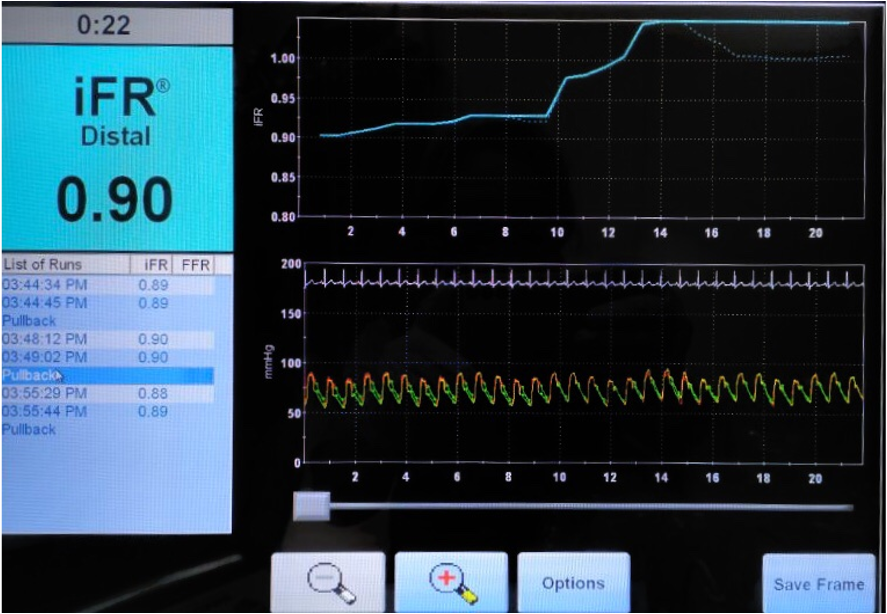
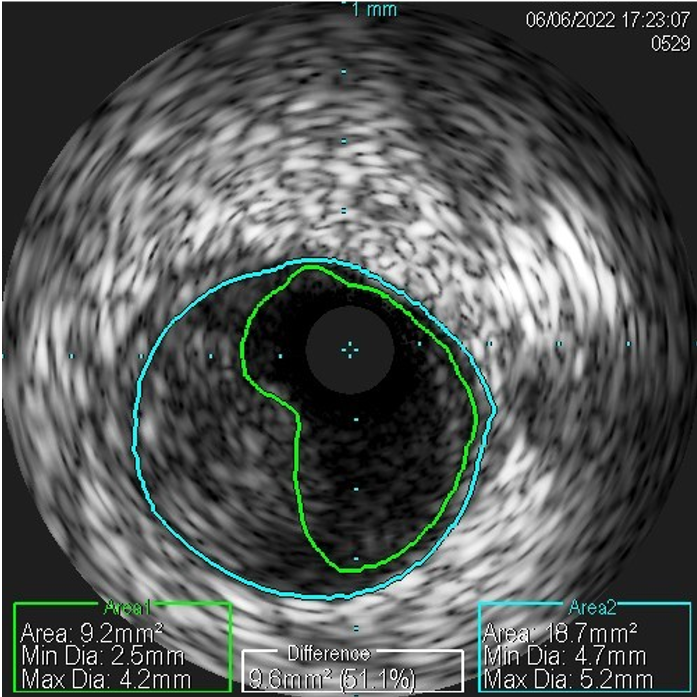
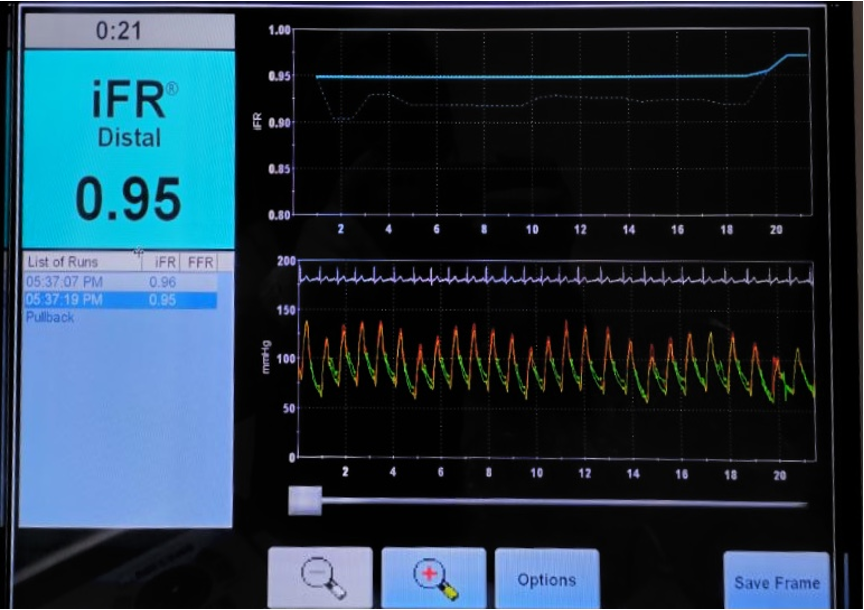
Physiologic lesion assessment (after 48 hours):iFR of LAD: 0.90iFR of RCA: 0.95IVUS of RCA: well-delineated vessel wall layers with well-formed thrombus without evidence of plaque erosion or rupture.

Physiologic lesion assessment (after 48 hours):iFR of LAD: 0.90iFR of RCA: 0.95IVUS of RCA: well-delineated vessel wall layers with well-formed thrombus without evidence of plaque erosion or rupture.

Interventional Management
Procedural Step
We proceeded with an early invasive strategy after ER assessment. Wall motion abnormality and ECG were consistent with an RCA culprit lesion. Angiogram showed an RCA with diffuse thrombus burden and a severely stenosed (80%) ostial LAD. Due to the diffuse thrombus burden of the RCA, the team decided to treat it with tirofiban drip. A stent was not placed at the ostial LAD since it was unlikely the culprit lesion and the functional significance of the LAD lesion is unknown. Instead, IVUS was planned for anatomic evaluation of the RCA thrombus and iFR for physiologic assessment of the LAD lesion. IVUS of the RCA and iFR of the LAD and RCA were done after 48 hours. A Verrata iFR pressure wire was advanced into the LAD, crossing the lesion at the proximal segment. Pullback was done with an iFR result of 0.90. IVUS of the proximal to distal RCA using Eagle Eye catheter via manual pullback showed well-delineated intima, media, and adventitia layers without evidence of plaque rupture or erosion with heavy thrombus burden but with good MLA of 9.2 mm2. iFR measurement was also done at the RCA using the same Verrata iFR pressure wire. The wire was then advanced into the RCA. Pullback was done with an iFR result of 0.95. The findings resulted in no further invasive intervention. Medical management was continued and the patient was eventually discharged.
Case Summary
This case shows the role of a physiology-guided approach in treating patients with acute myocardial infarction with multivessel disease. iFR can guide in the selection of which non-culprit lesion is warranted for angiographic intervention. IVUS capability of identifying the anatomic nature and character of the lesion provides additional information to the angiographer which can help in selecting the appropriate treatment strategy.


