Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-190
Successful Left Ventricular Unloading With Atrial Septal Stenting During Extracorporeal Membrane Oxygenation as a “Bridge to Heart Transplantation” in Patient With Severe Mitral Paravalvular Leakage
By Thitima Limjaroen, Supanee Sinphurmsukskul, Vorarit Lertsuwunseri, Suphot Srimahachota
Presenter
Thitima Limjaroen
Authors
Thitima Limjaroen1, Supanee Sinphurmsukskul1, Vorarit Lertsuwunseri1, Suphot Srimahachota1
Affiliation
King Chulalongkorn Memorial Hospital, Thailand1,
View Study Report
TCTAP C-190
STRUCTURAL HEART DISEASE - Others (Structural Heart Disease)
Successful Left Ventricular Unloading With Atrial Septal Stenting During Extracorporeal Membrane Oxygenation as a “Bridge to Heart Transplantation” in Patient With Severe Mitral Paravalvular Leakage
Thitima Limjaroen1, Supanee Sinphurmsukskul1, Vorarit Lertsuwunseri1, Suphot Srimahachota1
King Chulalongkorn Memorial Hospital, Thailand1,
Clinical Information
Patient initials or Identifier Number
P T
Relevant Clinical History and Physical Exam
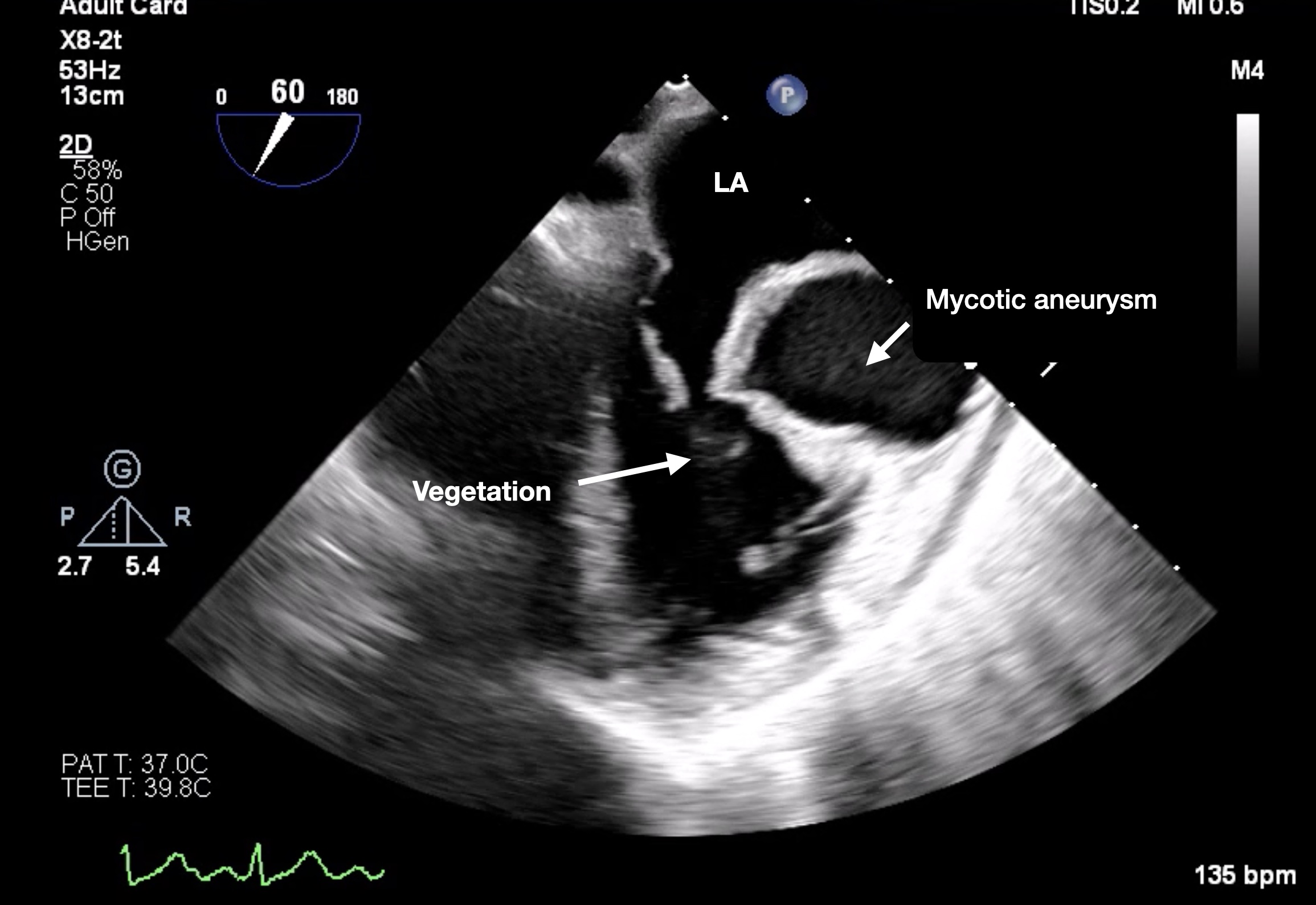
A 36-year-old man presented with 1 month of visual loss and fever. Transesophageal echocardiography (TTE) revealed multiple vegetations involving both mitral valve leaflets as well as perforated posterior leaflet, forming a giant mycotic aneurysm causing severe mitral regurgitation. He underwent mitral valve replacement after 2 weeks of antibiotic therapy.


Relevant Test Results Prior to Catheterization
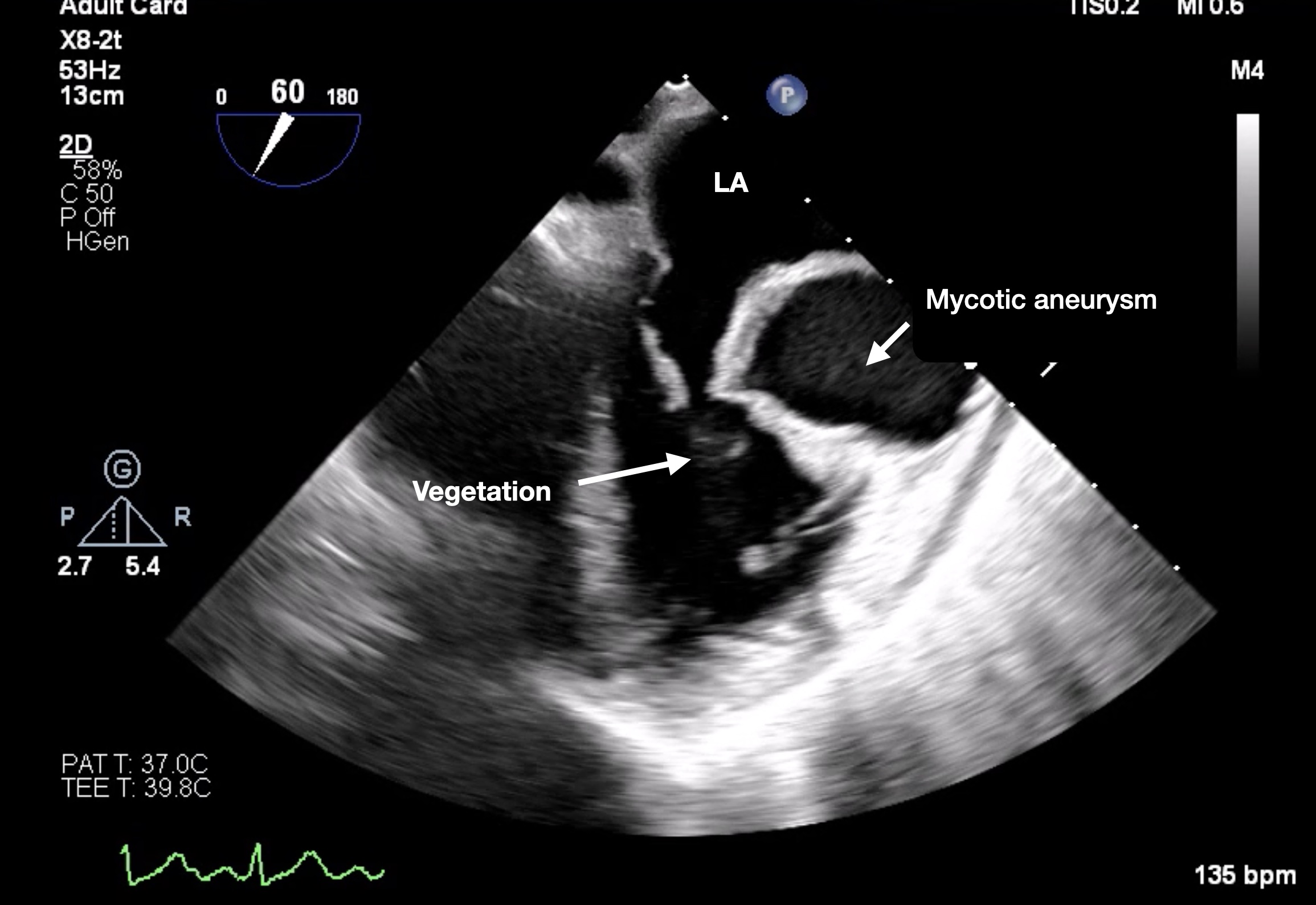
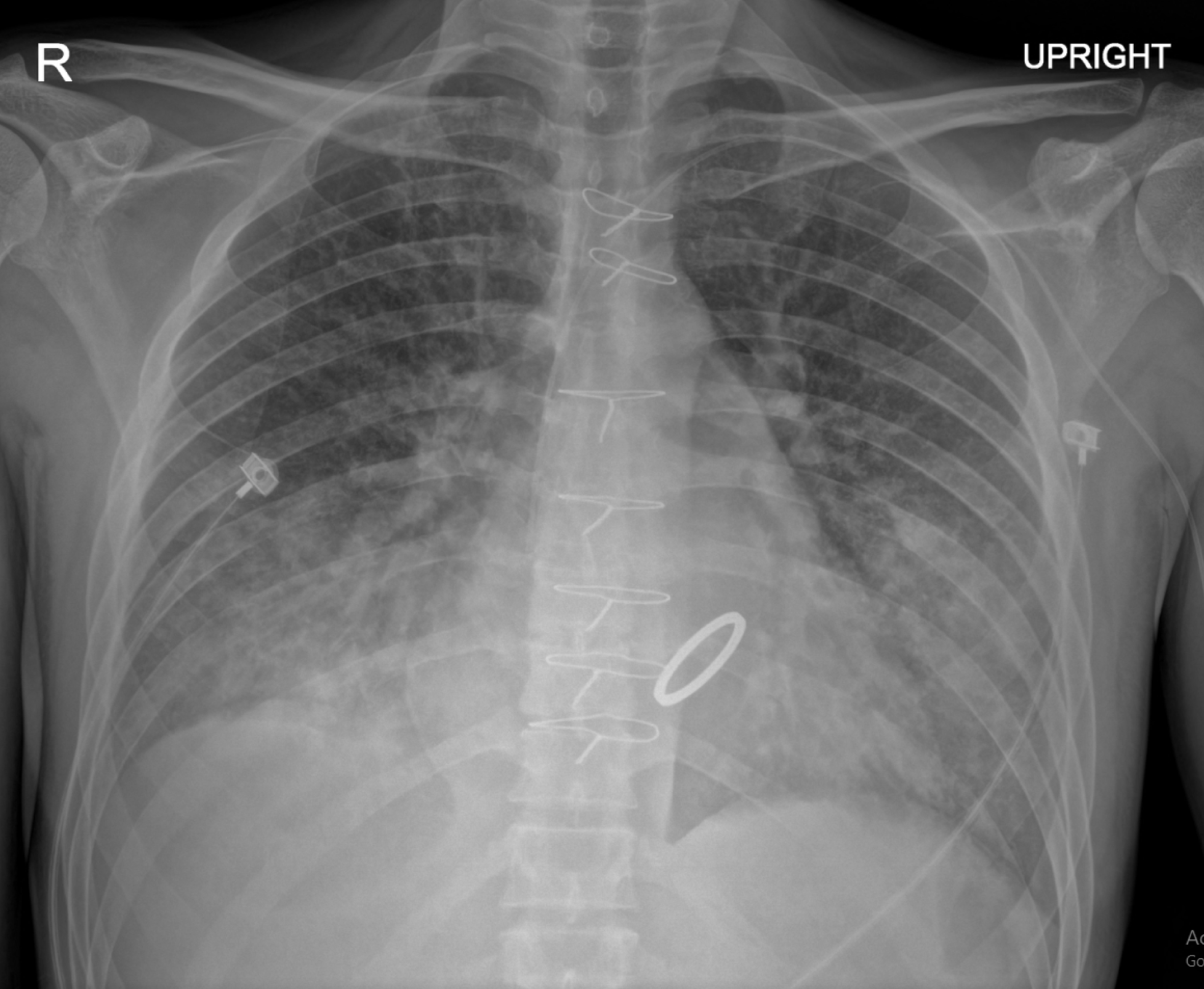
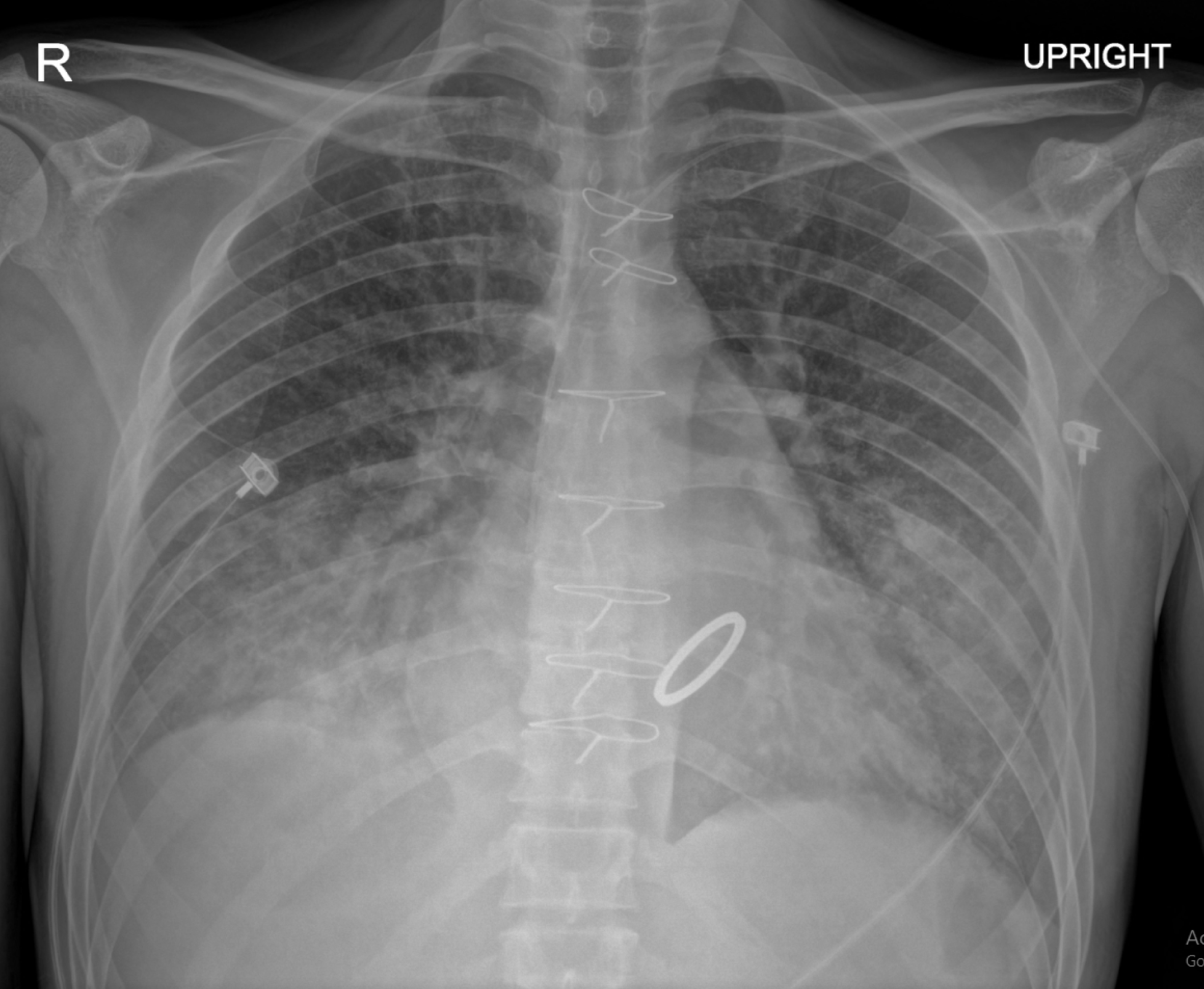
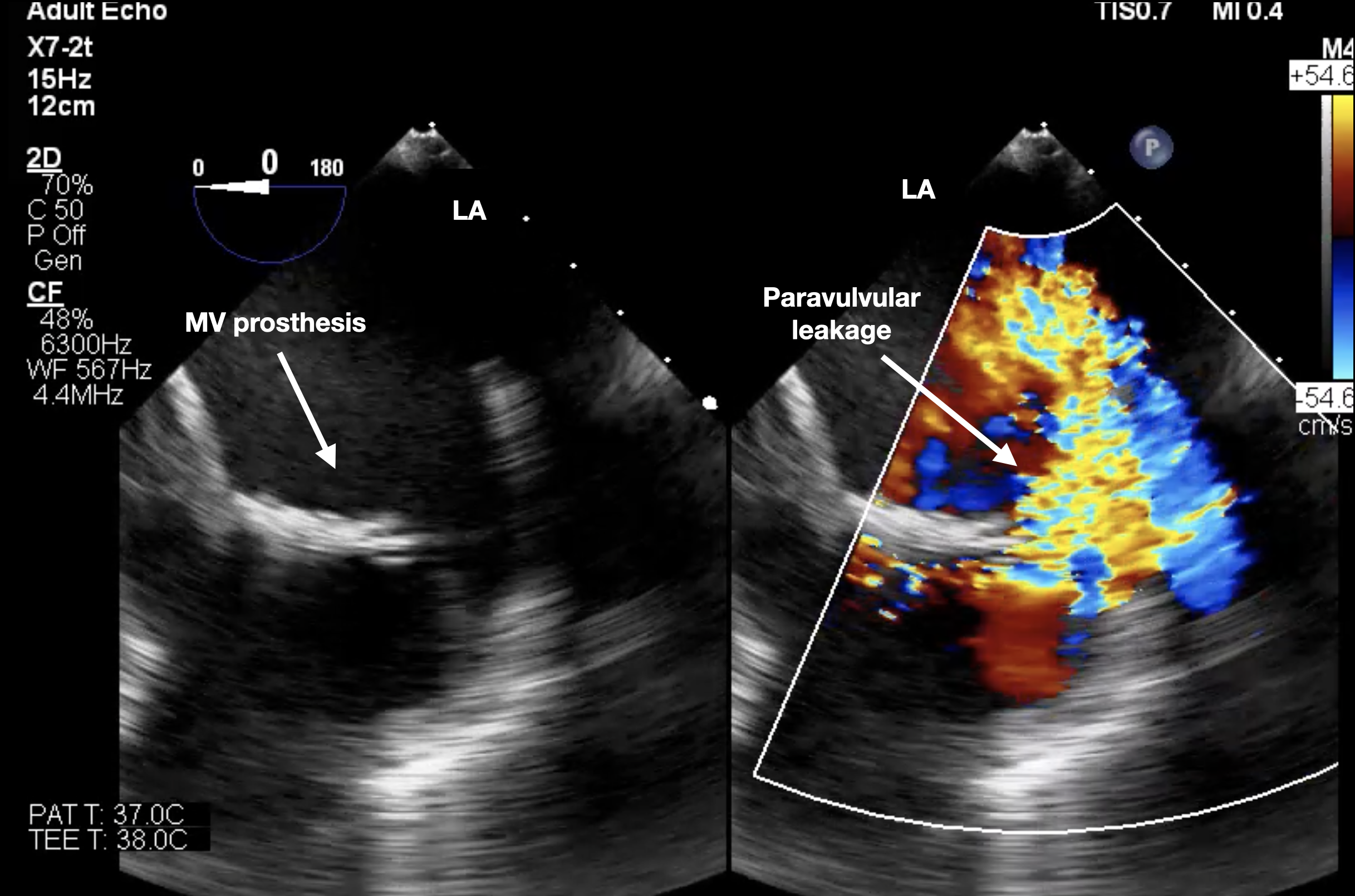
After 6 weeks postoperatively, he developed acute heart failure and cardiogenic shock. TEE showed paravalvular regurgitation, predominantly antero-lateral of the mitral valve prosthesis due to dehiscence of the commissures. Consequently, extracorporeal membrane oxygenation (ECMO) was initiated; however, he continued to have refractory pulmonary edema and echocardiographic evidence of left ventricular distension and aortic valve closure, indicating the need for urgent left heart unloading.
Relevant Catheterization Findings
Interventional Management
Procedural Step
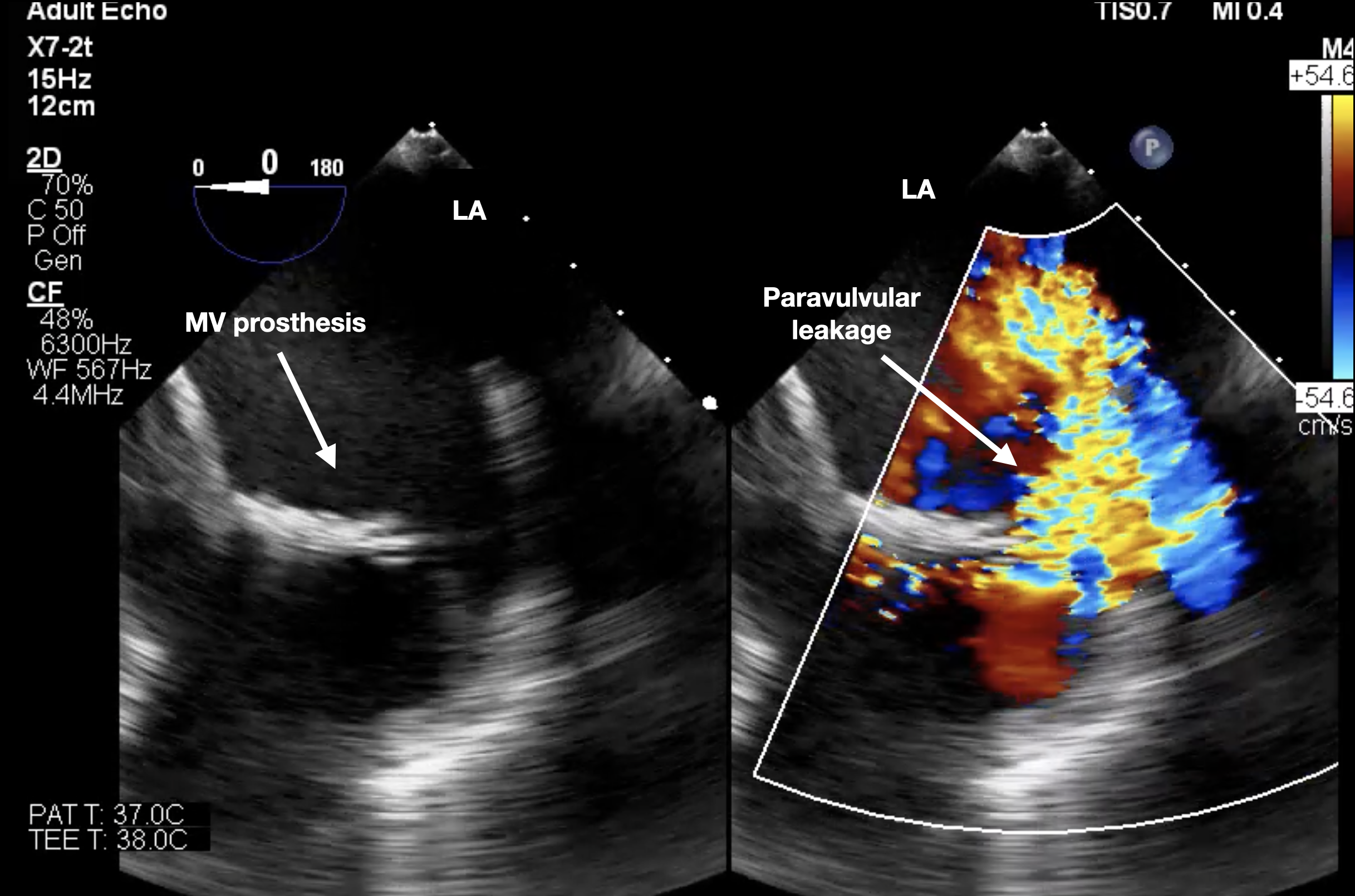
The atrial septal stenting procedure was done via the right femoral vein using a SL 0 Swartz TM braided transseptal guiding introducer sheath of 8.5 Fr. A 0.032" guidewire with a transseptal sheath was inserted, and the sheath tip was parked in the right jugular vein. A Brokenbrough septal puncture needle was introduced until its tip reached the end of the transseptal sheath. The arrow on the flange of the needle should point posteriorly and to the left at the 4–5 o'clock position. The transseptal sheath-needle assembly was moved toward the right atrium. TEE was used for the septal puncture site. Once the needle had passed through the left atrium, the transseptal sheath was advanced into the left atrium. Heparinization was done after confirming septal puncture, and then the needle was exchanged for a 0.035" wire. The left atrial pressure was 24/50/32 mmHg. The 10.0 mm x 19 mm stent Omnilink Elite was advanced across the interatrial septum. A contrast was used to confirm the location of the mid of the stent against the atrial septum. Once this point was reached, the stent-balloon assembly was fully unsheathed. After stenting, LA pressure was decreased to 17/46/25 mmHg. Doppler color flow imaging showed laminar flow across the stent. The patient's pulmonary edema improved after the procedure, and he underwent heart transplantation three weeks later. A gross examination of his heart revealed significant valvular dehiscence.


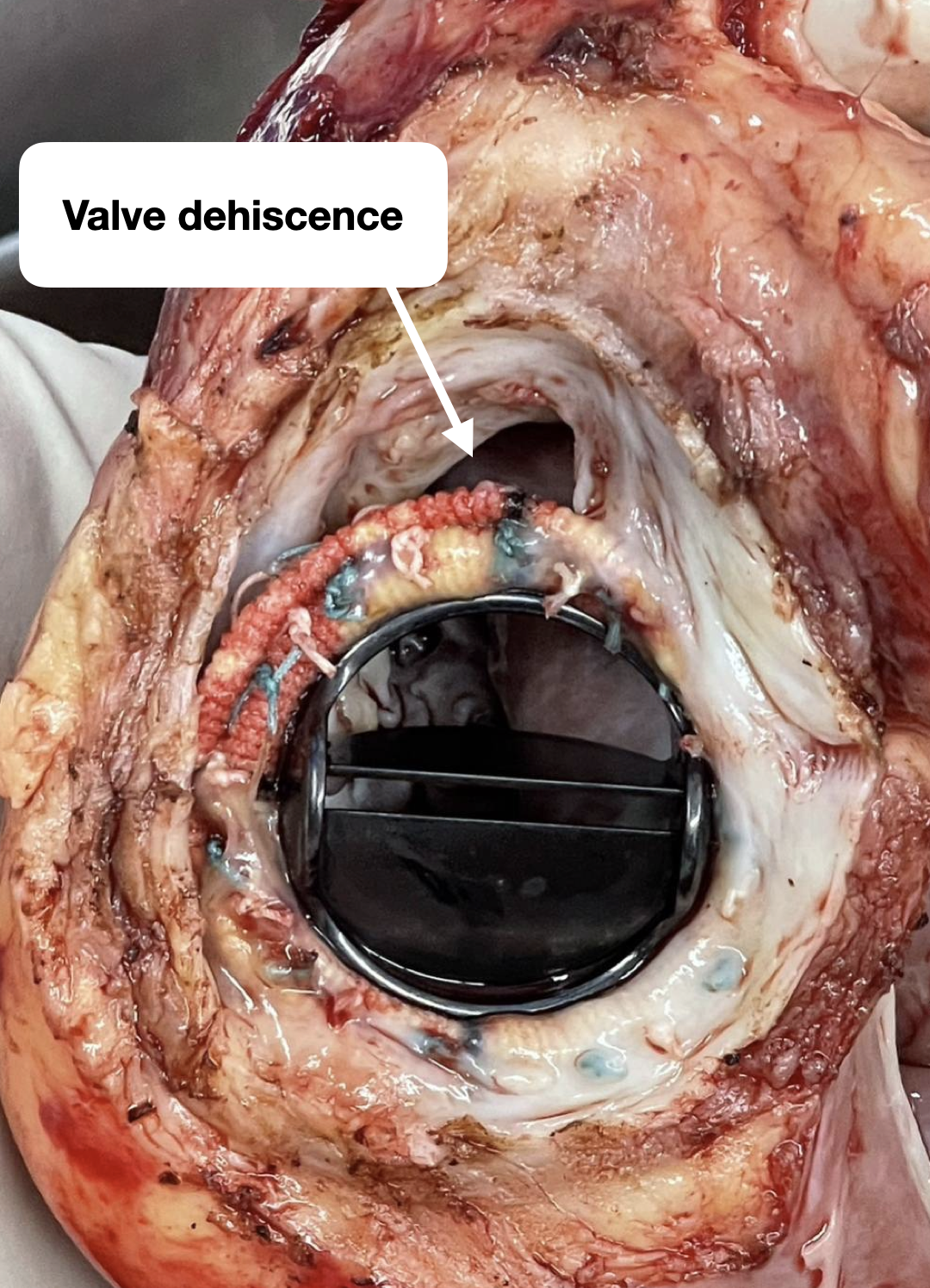


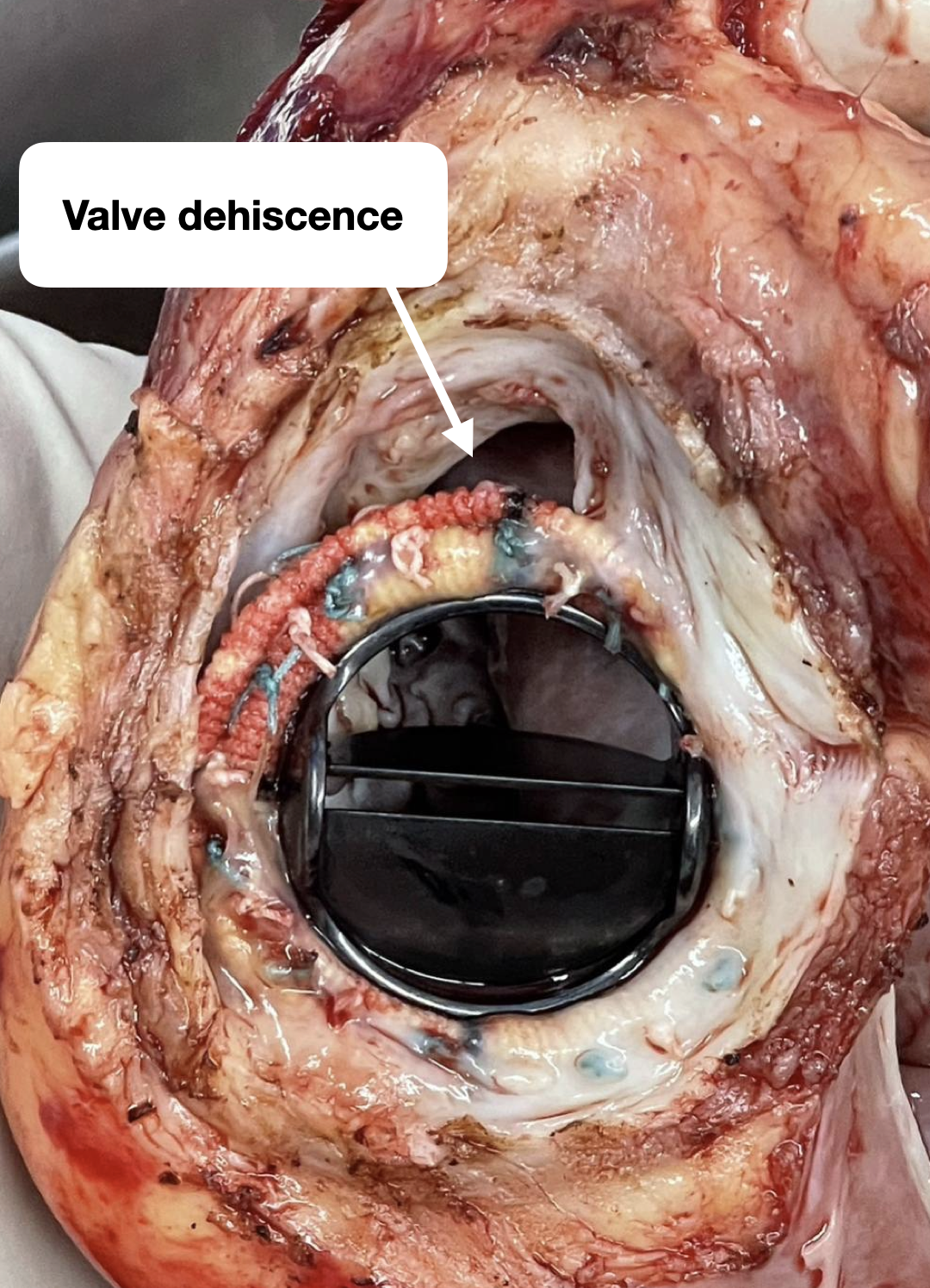
Case Summary
Persistent severe left ventricular dysfunction on ECMO causes increased wall stress, elevated myocardial oxygen demand, and increase left atrial pressure. Pulmonary edema limits ECMO support and requires left heart decompression. Atrial septal stent implantation offers an alternative approach for left heart decompression on ECMO as a supplement to ECMO as a bridge to heart transplantation.


