Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-093
Complex Calcified Left Main and LAD Percutaneous Coronary Intervention After CABG
By Azrina Abdul Kadir, Yu Ying Ong, Ng Kwang How, Hou Tee Lu
Presenter
Azrina Abdul Kadir
Authors
Azrina Abdul Kadir1, Yu Ying Ong2, Ng Kwang How3, Hou Tee Lu1
Affiliation
Sultanah Aminah Hospital, Malaysia1, Sultan Idris Shah Serdang Hospital, Malaysia2, University Malaya Medical Center, Malaysia3,
View Study Report
TCTAP C-093
CORONARY - Complex and Higher Risk Procedures for Indicated Patients (CHIP)
Complex Calcified Left Main and LAD Percutaneous Coronary Intervention After CABG
Azrina Abdul Kadir1, Yu Ying Ong2, Ng Kwang How3, Hou Tee Lu1
Sultanah Aminah Hospital, Malaysia1, Sultan Idris Shah Serdang Hospital, Malaysia2, University Malaya Medical Center, Malaysia3,
Clinical Information
Patient initials or Identifier Number
Mrs RAK
Relevant Clinical History and Physical Exam
Mrs RAK, a 45-year old lady who presented with fluid overload symptoms with ankle swelling, ascites and exertional dyspnea on 14/6/2022. She has a background of diabetes mellitus, hypertension, ischemic heart disease with previous CABG for triple vessel disease with LIMA to LAD, SVG to PDA and LCX in May 2021. She has history of unstable angina 4 months after CABG and graft study showed graft stenoses which were treated medically. She has heart failure and liver cirrhosis with portal hypertension. Clinically she is overloaded with peripheral oedema, ascites and bibasal crepitations.
Relevant Test Results Prior to Catheterization
ECG showed Q waves in the anterior leads with poor R wave progression. Troponin was not elevated but pro-BNP was >9000 pg/ml. She has acute kidney injury with Creatinine 124 umol/L and has congestive hepatitis with ALT 76 U/L and ALP 224 U/L , haemoglobin 12.6 g/dL. ECHO showed LVEF 45-50%. She was started on on IV Frusemide and paracentesis for gross ascites.
Relevant Catheterization Findings
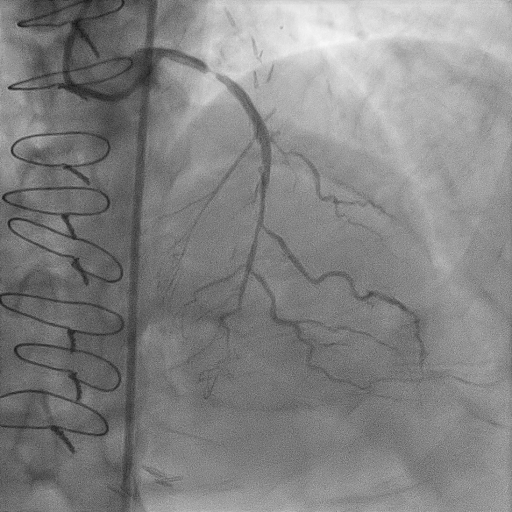
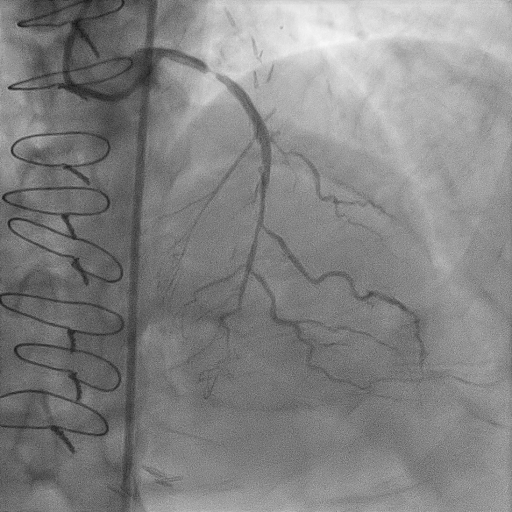
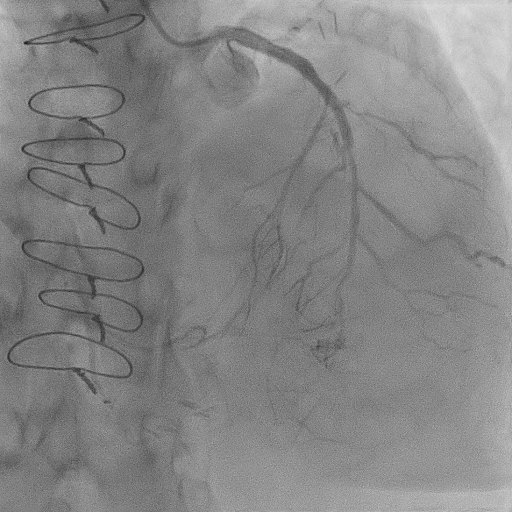
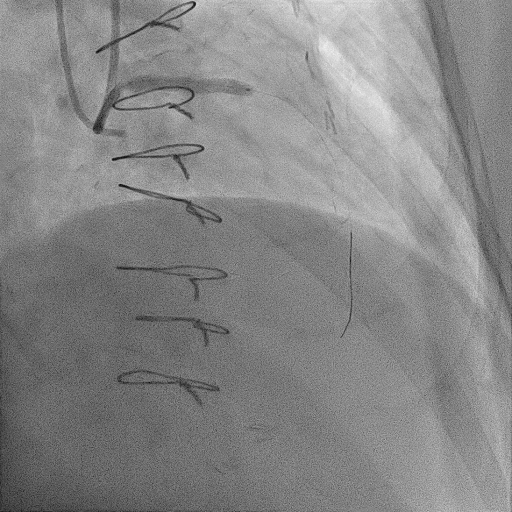
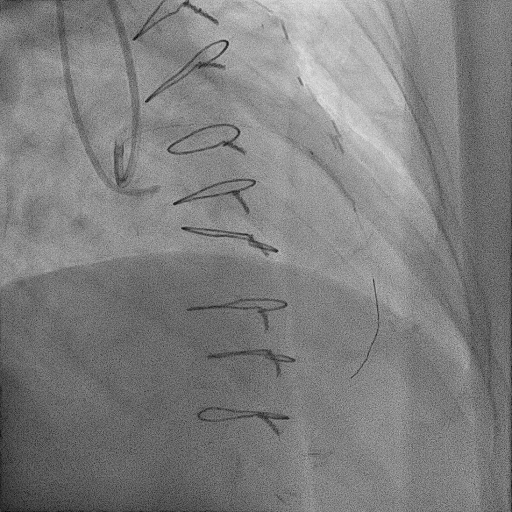
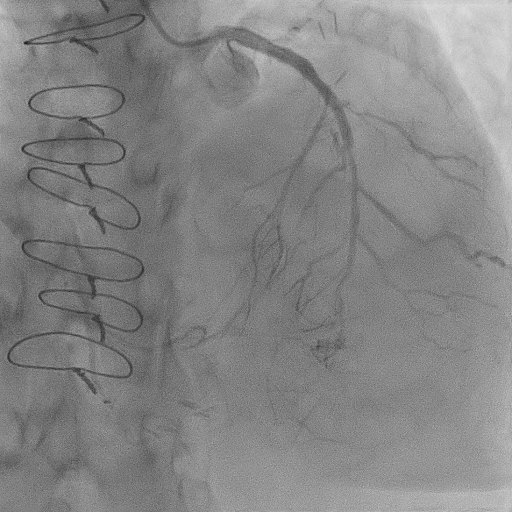
She underwent graft study which showed distal left main stenosis 90%, ostial LAD 90%, ostial LCX CTO, 80% stenosis of LIMA to LAD at anatomotic site, 80% stenosis at distal SVG to PLV and patent SVG to PDA which collateralised the distal LCX.
Interventional Management
Procedural Step
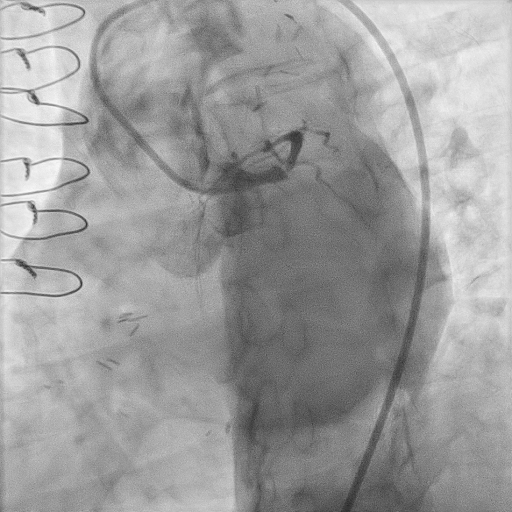
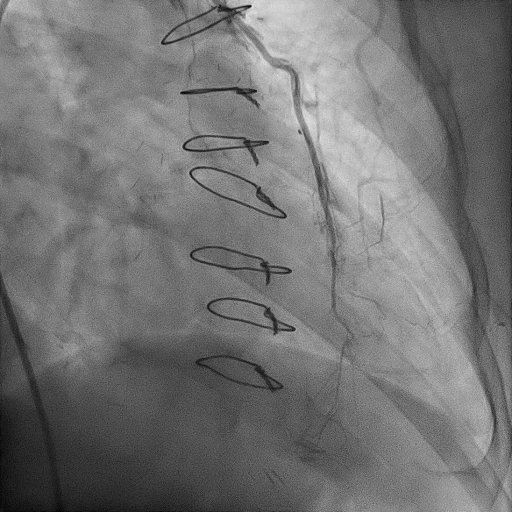
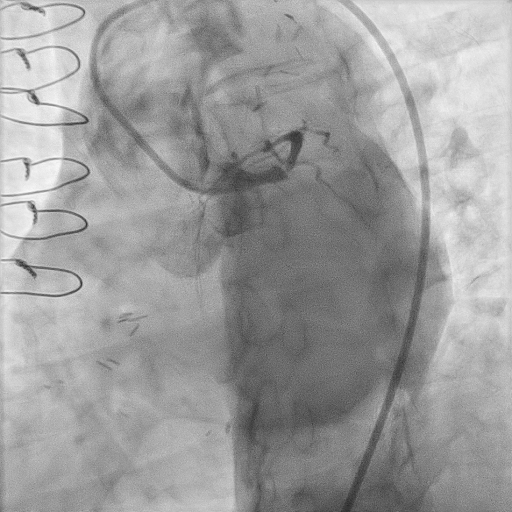
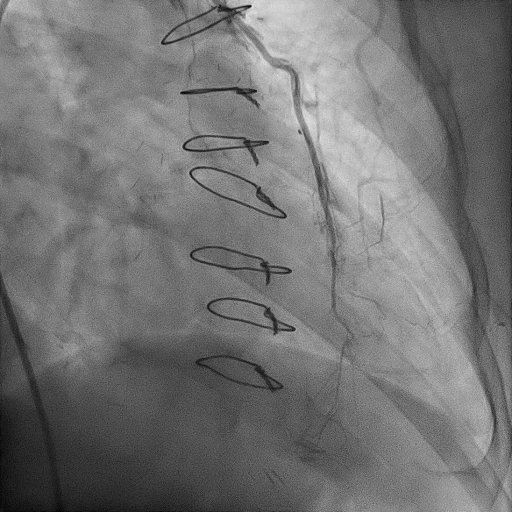
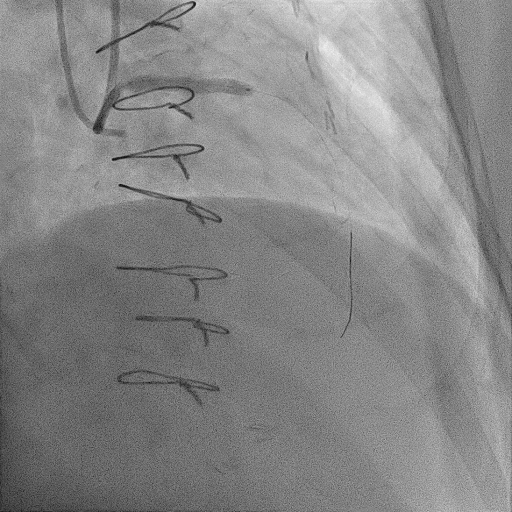
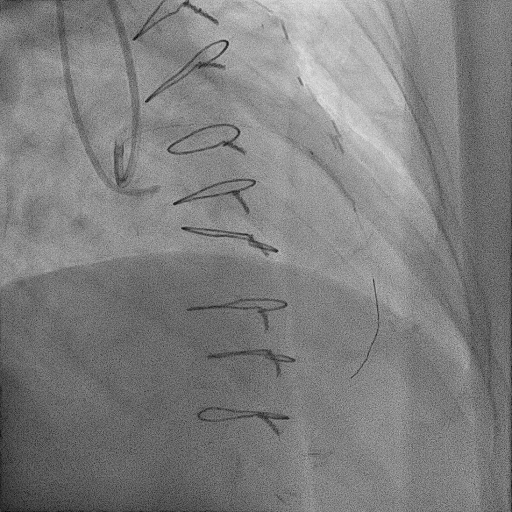
PCI was performed via 7Fr right femoral artery(RFA) and 6Fr right radial artery(RRA). Total of 10,000u intracoronary heparin given. Left coronary ostium was engaged with 7Fr EBU 3.5 and right ostium with 6Fr JR4. Wired to distal LAD with runthrough floppy and predilated ostial LAD with SC 1.2 x 12mm. Rotational atherectomy was performed to proximal LAD (pLAD) with 1.5 burr at 180,000 RPM for 2 runs. IVUS performed and revealed 270 degree calcium arc. Predilated pLAD with NC 2.5 x 12 mm then Wolverine 3.0 x 10 mm and NC 3.5 x 8 mm. Prior to stenting across LAD to left main, we decided to attempt PCI to ostial LCX with Fielder XT-R through microcatheter Mizuki, but was unsuccessful and escalated to Miracle wire but failed and procedure abandoned. Stented proximal LAD to ostial LM with DES Promus Premier 4.0 x 28 mm and postdilated stent with NC 4.5 x 8 mm. Stent was optimized with IVUS guidance. We then placed drug coated balloon (DCB) In.Pact Falcon 2.0 x 20 mm at mid LAD. End result was good, TIMI 3 flow with no dissection. We decided to PCI SVG to PLV by using BMW wire to PDA and PLV with Fielder XT-R with microcatheter Mizuki. We then tried to advance SC 1.2 x 12 mm balloon to ostial PLV but was unsuccessful and procedure abandoned. Total procedural time was 3 hours and 3 minutes with 260 ml of contrast. Patient was discharged well 5 days after the procedure due to mild worsening of kidney function which resolved spontaneously. Relook CAG 4 months later showed patent LM to pLAD stent.
Case Summary
Small and diffuse coronary artery disease poses challenging and limited revascularization options due to high rate of target vessel failure. Diffuse, multivessel, occluded and presence of collateral vessels are among significant independent predictors for target vessel revascularization after CABG, which was illustrated in this case in which graft failure was seen only after 5 months of CABG. Patient stabilization and optimization pre and post-PCI are important to ensure the success and excellent clinical outcome of the procedure. Intravascular imaging such as IVUS plays an important role in the assessment of the extent and severity of calcification, vessel size and stent optimization especially in the left main lesion. Drug coated balloon is an attractive option with growing evidence for diffuse and small vessel disease.


